Article
Dermascope vs Dermatoscope: Exploring the Diagnostic Power beyond the Magnifying Glass
Dermascope vs Dermatoscope What is a dermatoscope?Dermatoscope, also know as dermoscope or epiluminescence microscope. It is a useful and dependable hand-held microscope device for skin examination, such as melanoma, alopecia areatap, onychosis,etc. This device allows sharp examination of skin structure by high quality magnification and super lighting system. Under dermatoscope, specific patterns and features of…
Dermascope vs Dermatoscope
What is a dermatoscope?
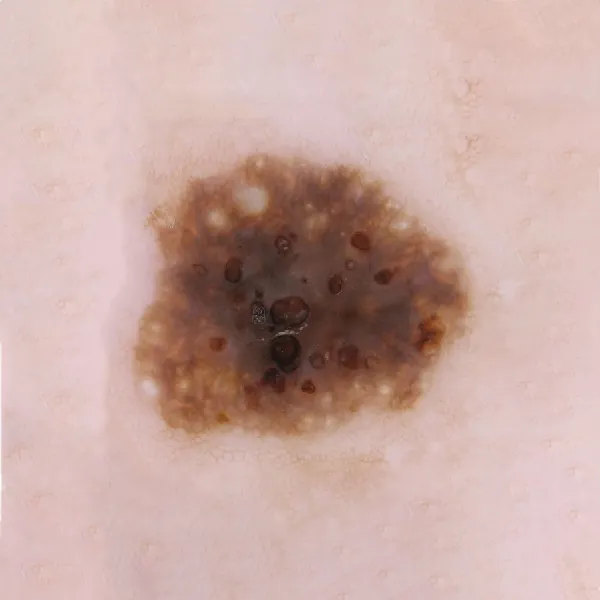
Dermatoscope, also know as dermoscope or epiluminescence microscope. It is a useful and dependable hand-held microscope device for skin examination, such as melanoma, alopecia areatap, onychosis,etc. This device allows sharp examination of skin structure by high quality magnification and super lighting system. Under dermatoscope, specific patterns and features of skin can be showed clearly and precisely.
Dermascope vs dermatoscope: dermoscope is the synonyms of dermatoscope.
What is the use of dermatoscope?
Dermatoscope can record the images for comparison in future. What’s more, it can monitor and assess the structure of the reticular dermal depth. The basic principle of dermatoscope is to take a translucency of the skin lesion so that it can be studied at high magnification to visualize subtle features.
Dermatoscope can magnify the outer layer of the skin greatly. Under dermatoscope, skin doctors can inspect skin colors, shapes, sizes and patterns more precisely to help distinguish and diagnose a variety of skin situations.
Skin doctors can use dermatoscope to examine situations which not related to lesions, such as melasma, hair losss, scabies, etc.
With the help of dematoscope, doctors can identify non-cancerous lesion, including dermatofibromas, warts and so on.
Dermatoscope can also help to diagnose cancerous lesions, like basal cell carcinoma, nodular melanoma, melanoma, etc.
Information from dermatoscope helps doctors to evaluate whether skin disease is progressing and whether treatment is needed or not. And it enhance doctor’s confidence in diagnosing skin situation and also greatly saves doctor’s time.

What are the types of dermatoscope?
There are many types of dermoscopes, each designed for a specific use and function. Here are the key types:
• Hand-held portable dermatoscope: This is a common type and it is often used due to its convenience and mobility. It typically includes a transparent light source and an amplifying optical device, usually providing a magnification of about 10-fold.
• Stationary Mounted Type: This kind of dermatscope is designed to capture whole body images in one shot. They are typically integrated with image analysis algorithms to generate a three-dimensional model of the human body and use artificial intelligence to label and analyze lesions.
In addition, dermatoscope have different models of operation, such as unpolarized light contact, polarlized light contact, polarlized non-contact, etc.
• Unpolarized light, contact: Unpolarized light is a natural light with intrinsically incoherent and it has an electric field that oscillates in all directions. It can provides information for superficial skin.
• Polarized light, contact: Polarized light is intrinsically coherenn and it has an electric field that oscillates in only one direction. Polarlized light contact can reveal the depth of skin structures.
• Polarized light, non-contact: As its name, skin can be inspected without contact. It is very suitable especially in sensitive area. By using polarized light, it can eliminate the reflection and surface glare of skin to show the dermis structures of skin.

What are the clinical effects of dermatoscope?
In the field of dermatology, the clinical effects of using a dermatoscope is of great significance. Especially in the monitoring and diagnosis of skin lesions. Here are some of the main advantages:
• Enhanced Diagnosis: Dermatoscopy helps dermatologists to identify pigmented skin lesions more accurately, which can avoid some unnecessary surgery or skin biopsies.
• Monitoring Changes: Dermatoscope helps dermatologists to detect moles and other pigmented skin lesions over time for any changes, which is very important for early monitoring of skin cancer.
• Non-Invasive: The whole procedure is painless and non-invasive, and it is suitable for all skin types and ages.
• Visualization of Subsurface Structures: Dermatoscopy offers a amplifying view of the dermoepidermal junction, epidermis, and papillary dermis, which can not be saw by the naked eye.
• Digital Documentation: Images captured by the dermatoscope can be digitally recorded for sequential monitoring or storage,helping to observe suspicious lesions carefully.
These clinical effects contribute to the early examination and treatment of skin cancers such as basal cell carcinoma and melanoma, as well as in the treatment of other skin diseases.
Detection of melanoma with dermatoscope
Dermatoscopy is a noninvasive, aided instrument by dermologists used for the examination of various skin lesions, like melanoma. Dermascope vs dermatoscope: Dermoscopy is performed with a handheld device called a dermatoscope.
The detection of melanoma with dermatoscope is a critical process that involves identifying specific patterns and structures that are indicative of the disease. Here are some key points regarding melanoma detection with a dermatoscope, such as early detection, specific features, improved accuracy.
What’s another name of dermatoscope?
A dermatoscope is also known by several other names, including: deromscope, dermoscopy, dermatoscopy, Epiluminescence Microscopy, Epiluminescence Microscopy, Incident Light Microscopy and so on. Dermascope vs dermatoscope, deroscope is another name of dermatoscope.
Dermatoscope vs Magnifying Glass
Do dermatologists use magnifying glass?
Yes, for a more general examination of the skin, dermatologists may use simple magnifying glass to inspect the skin. And a magnifying glass is usually used to show a magnified image of objects.
Dermatoscope vs magnifying glass:While a dermatoscope is a specialized tool that connects physic and optic. It can reveal the dermis and epidermis of skin clearly through eliminate the light glare and reflection of skin.Dermascope vs dermatoscope: Dermoscope is also know as dermatoscope, is a valuable and dependable device for dermatologists.
What is the difference between dermatoscope and magnification?
Dermatoscope vs magnifying glass:Dermatoscope (Dermoscope) is a valuable aid device used by skin doctors to examine skin lesions with more details. It combines illumination with magnification to release a clear view of underground structures that are invisible to the routine examination by naked eye. Dermatoscope vs magnifying glass, here’s the differences as below:
• Magnification: Usually it means to use lenses or digital technology to enlarge an image. It does not contain a light source, nor does it display subsurface of the skin in details.

• Dermoscopy: While dermoscopy is working, it magnifies the surface of the skin, at the some time, it also illuminates the skin with specific types of light. So it greatly enhance the view of skin structures and patterns under the surface, which is essential for diagnosing skin diseases such as melanoma.
In essence,Dermatoscope vs magnifying glass, magnification can amplify objects and make it looks larger. But the function of dermoscopy is far more than this. It can provide a more comprehensive view by combining magnification and illumination, helping skin doctors to diagnose more accurately.






















