Article
Dermatoscope of Basal Cell Carcinoma
Dermatoscope of Basal Cell Carcinoma Basal cell carcinoma (BCC) is the most common skin cancer in humans. In all over the world, the incidence of basal cell carcinoma accounts for at least 80% of skin cancers besides melanoma and 32% of all cancers. BCC mainly occurs in Caucasians and is very rare in people with…
Dermatoscope of Basal Cell Carcinoma Basal cell carcinoma (BCC) is the most common skin cancer in humans. In all over the world, the incidence of basal cell carcinoma accounts for at least 80% of skin cancers besides melanoma and 32% of all cancers. BCC mainly occurs in Caucasians and is very rare in people with dark skin. The incidence of BCC is increasing globally. The number of reported cases in the United States has also steadily increased, with an estimated 3.6 million Americans diagnosed with BCC each year.
Basal cell carcinoma is caused by abnormal, uncontrolled growth of basal cells. Due to cell carcinomas grow slowly, so most of them are curable. Although it is rarely fatal, basal cell carcinoma can be highly destructive and destroyed in local tissues if treatment is inadequate or delayed. It needs to be detected early and treated aggressively so that the damage caused by basal cell carcinoma is minimal. So understanding the genesis, risk factors, and warning signs of basal cell carcinoma can help us detect them early. Let basal cell carcinoma get early treatment and cure.
What is basal cell carcinoma?
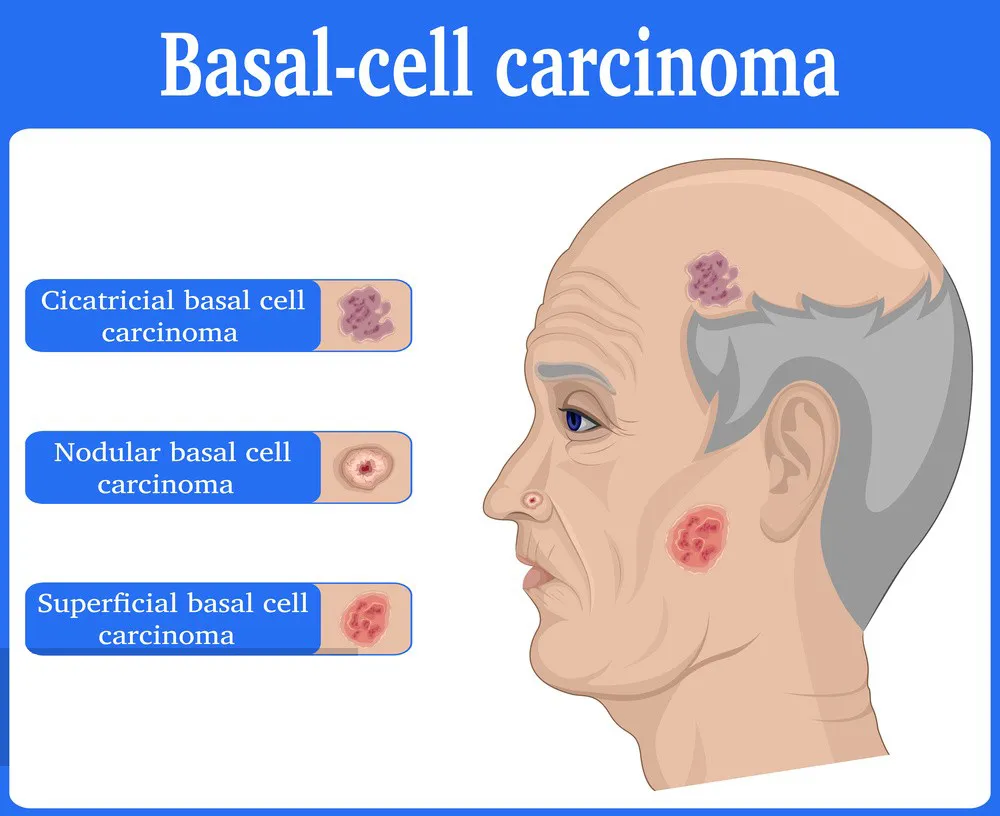
Basal cell carcinoma (BCC) is a kind of skin cancer that starts in the basal cells, which are located in the deepest layer of the epidermis. Basal cell carcinoma occurs most often when exposure to ultraviolet (UV) radiation from the sun or indoor tanning triggers DNA damage that causes changes in the basal cells of the outermost layer of the skin, leading to uncontrolled growth. Therefore, basal cell carcinoma most often occurs in areas of the skin that are exposed to a lot of strong sunlight. Exposed areas like the face, neck, arms, legs, etc. Otherwise, it is rarely on the palms and soles of the feet. Basal cell carcinoma usually appears as small shiny bumps or pink growths on the skin.
What are the clinical features of basal cell carcinoma?
Basal Cell Carcinoma (BCC) is the most common skin cancer and has specific clinical features, including:
- Chronic growth: Basal cell carcinomas generally grow slowly, usually over months to years. Lesions of basal cell carcinoma usually enlarge gradually over months to years.
- Rare transfer: Basal cell carcinoma rarely transfer far away, but it can invade surrounding tissues and organs if not treated promptly.
- Presentation: BCC usually appears as skin colored, pink, or pigmented mass that may be accompanied by bleeding, erosion, or ulcers.
- Marginal features: The margins of basal cell carcinoma are usually well-defined, semi-circular or oval in shape.
- Central depression: BCC often has a central depression or ulcer.
- Common Sites: Basal cell carcinoma is most common in areas with high exposure to ultraviolet light, such as the face, scalp, neck and back.

Basal cell carcinoma dermoscopy
What is dermoscope?
Dermoscope is also known as transmittance microscope of skin.It can remove the reflection from the surface of skin lesions through polarization or nonpolarized mode, and observe subtle pigmentation loss deep in the skin that is invisible to the naked eye, as well as changes in skin texture and blood vessel structure. Under dermoscopy, skin doctors can comprehensively
detect and diagnose the skin lesions of skin diseases. Just like a physician’s stethoscope, dermoscope is a non-invasive examination tool commonly used in dermatology.
Such as dermoscope can help detect early cancers that is difficult to detect with the naked eyes. Especially, dermoscopy is useful for observing key features like lesion boundaries and vascular distribution of basal cell carcinoma. So that dermatologists can diagnose and treat basal cell carcinoma accurately and timely. Basal cell carcinoma dermoscope means greatly in medical field.
What are the characteristics of basal cell carcinoma dermoscopy?
There are some key characteristics of basal cell carcinoma dermoscopy like belowing:
- Border: Irregular edge
- Color: Translucent, pearl white, skin color or pink
- Shape: Lumps, papules, spots, balls, scars
- Distribution: Various morphological vascular distribution, such as linear and dendritic
- Others: Localized ulceration, basal cells may ooze, itch, bleed or crust

It’s important to note that everyone’s features of basal cell carcinoma dermoscopy may look different. Dermoscopy indeed plays a very important role in the analysis and diagnosis of basal cell carcinoma.
Application of basal cell carcinoma dermoscopy
A dermoscope is a microscope used to examine skin lesions. In the diagnosis and treatment of basal cell carcinoma, basal cell carcinoma dermoscopy is widely used in the following aspects:
Early diagnosis: By magnifying and permeating the details of skin lesions, dermoscopy allows doctors to identify the characteristics of basal cell carcinoma more clearly, so that lesions can be detected and treated as early as possible. It can help doctors accurately detect and diagnose basal cell carcinoma at its early stage.
Treatment monitoring: For patients who have already been diagnosed with basal cell carcinoma, dermoscopy can be used to monitor the whole changes in the lesion at any time.
Feedback comparison: Physicians can compare dermoscopic images at different time to assess the effectiveness of treatment and then determine whether treatment needs to be adjusted.
Surgical aid: When surgically treating basal cell carcinoma, dermoscopy can help the doctor confirm the boundaries and depth of the lesion, not only allowing for more precise removal of the tumor but also less damage to healthy skin.
Precautions for basal cell carcinoma dermoscope in daily life
Dermoscopy is a necessary and reliable technique for skin analysis in daily life, while there some main matters need attention:
- Correct operation: Know how to use the dermoscope correctly when detect the basal cell carcinoma. In addition,make sure to clean and disinfect the equipment to avoid cross infection or the spread of bacteria before using the dermoscope.
- Proper light environment: Ensure the working environment of the dermoscope is under appropriate light, too strong or too weak light both will reduce the effect of basal cell carcinoma dermoscopy.
- Photo documentation: Know how to take photos and keep records for later analysis and evaluation, and comparison of before and after the basal cell carcinoma dermoscopy.
- Communicate with dermatologist: While a dermoscope can help you detect skin lesions better, any suspicious skin lesions noted, please have them evaluated by a dermatyologist.
It is very helpful to use basal cell carcinoma dermoscopy at its early stage. Dermoscopy plays a significant role in the diagnosis, treatment, and monitoring of basal cell carcinoma. Dermatoscope not only improves the accuracy of diagnosis, guides treatment decisions, but also enhance confidence for skin doctors and patience. People should pay more attention to self-examination of basal cell carcinoma dermoscopy regularly.






















