Article
Dermoscopy Examination
Dermoscopy examination is the examination of a patient’s skin using a dermatoscope. It essentially allows the use of a skin microscope that magnifies dozens of times, through optical magnification and polarization patterns, so that the deeper layers of the skin can be viewed. In the diagnosis of skin diseases, dermoscopy can help doctors observe subtle…
Dermoscopy examination is the examination of a patient’s skin using a dermatoscope. It essentially allows the use of a skin microscope that magnifies dozens of times, through optical magnification and polarization patterns, so that the deeper layers of the skin can be viewed. In the diagnosis of skin diseases, dermoscopy can help doctors observe subtle pigment and vascular structural changes that cannot be observed with the naked eye, thus providing a comprehensive understanding of the skin lesions of skin diseases. For example, dermoscopy can observe the typical features of basal cell carcinoma, such as uneven pigmentation, dilated capillaries, and scaling, which can help doctors determine whether it is basal cell carcinoma.
Basic Principles of Dermoscopy Examination
The IBOOLO DE-4100 and DE-3100 Dermatoscopy Optical Magnification Systems magnify skin lesions up to ten times through a combination of multiple glass lenses. Both dermatoscopes utilize the principle of polarized light, which enhances the collection of transmitted light by adjusting the direction of light polarization to reduce the interference of reflected light from the skin surface. This technology allows the dermatoscope to penetrate deep into the skin tissue and observe the structure and characteristics of the epidermis and dermal papillary layers.

Dermoscopic Features of Basal Cell Carcinoma
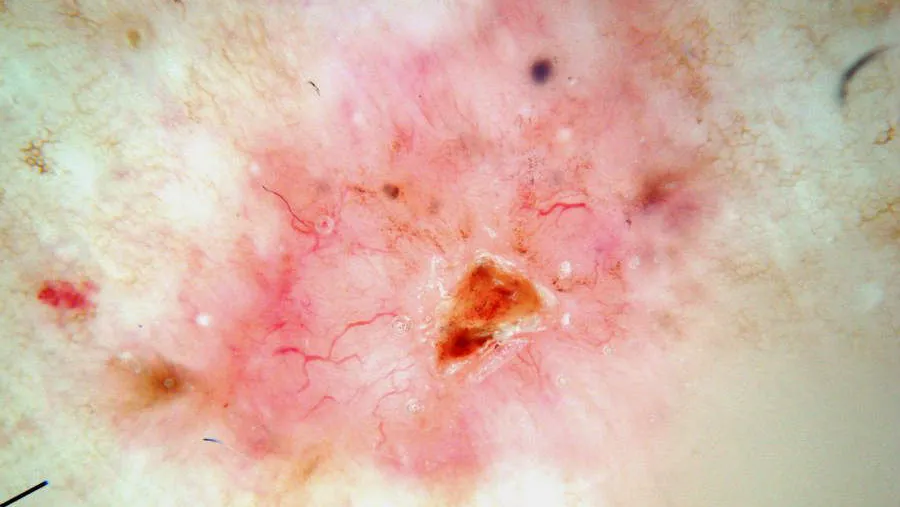
Dermoscopy can acutely capture subtle color distinctions and changes in skin lesions, and therefore, dermoscopy has significant advantages in the diagnosis of skin diseases such as pigmented nevi, malignant melanoma and basal cell carcinoma. The following is an example of dermoscopic examination of basal cell carcinoma.
Dermoscopic features of basal cell carcinoma mainly include the following aspects:
Large blue-gray ovoid nests: this is one of the classic dermoscopic features of pigmented basal cell carcinoma, which is manifested by the appearance of multiple blue-gray ovoid structures of varying sizes in the lesion area.
Multiple blue-gray spherules: these spherules are usually distributed in a non-aggregated fashion and are another classic dermoscopic feature of basal cell carcinoma.
Spoke-like areas: Spoke-like areas appear as structures radiating from the center of the lesion to the periphery.
Importance of Dermoscopy Examination for Early Detection of Basal Cell Carcinoma
Basal cell carcinoma, a kind of malignant tumor originated from basal-like cells, is one of the most common skin malignant tumors, and its incidence rate is very high.BCC grows slowly but has the characteristic of local infiltrative growth, which is capable of destroying tissues and organs, and even threatens the patients’ lives in serious cases.
Dermoscopy plays a crucial role in the early detection of basal cell carcinoma. Dermoscopy examination can quickly capture many typical features of basal cell carcinoma, such as dendritic blood vessels, superficial short capillary dilatation, bleeding ulcers and so on. In addition, dermoscopy can also assess the infiltration depth and scope of basal cell carcinoma, which provides an important basis for the formulation of treatment plan.
IBOOLO Dermatoscope
IBOOLO has different series of dermatoscopes that offer different options for dermatoscopic examination. DE-200, DE-300 and DE-400 are pocket dermatoscopes that are compact and can be carried around. The DE-200, DE-300 and DE-400 are handheld dermatoscopes that can be used to view lesions directly through a window or to connect to a cell phone via a magnet. the DE-200, DE-300, and DE-400 are relatively inexpensive and have polarization, making them ideal for those who require only basic dermatoscopic functionality. the DE-3100 and DE-4100 are relatively inexpensive and have polarization, making them ideal for those who require only basic dermatoscopic functionality. The DE-3100 and DE-4100 are more expensive and have a variety of illumination sources and brightness adjustments, making them ideal for professionals.
Dermoscopy Procedure
The following is the procedure for a dermoscopy from start to finish. First, the surface of the patient’s skin that needs to be examined needs to be cleaned to ensure that it is dry and free of oil and dirt. Next, the probe of the dermatoscope is attached to the skin surface that needs to be observed. Keep the distance between the probe and the skin, adjust the focus until the image is clear to start observation. You can connect the dermatoscope to your cell phone to save photos of skin lesions. The doctor can judge the disease based on the skin pigmentation and blood vessel changes in the dermatoscope window, and suggest the appropriate treatment plan for the patient.

Advantages of the Dermoscopy Procedure
The entire process of dermoscopy usually takes less than 10 minutes, making it a quick and easy procedure. It enables doctors to obtain detailed information about the skin surface in a short period of time. Moreover, dermoscopy is a non-invasive and non-invasive diagnostic method that does not cause any damage to the skin or any discomfort to the patient, making it easier for the patient to accept this method of examination.
Dermoscopy Examination and Specialized Training
Dermoscopy is only an examination tool to provide professionals with a good viewing field. The final result of the examination still largely depends on the experience as well as the knowledge of the doctor. Therefore, it is important for healthcare professionals to receive systematic training on the basic principles of dermoscopy, its operation and the dermoscopic features of common skin diseases. There is a wide variety of skin diseases and new diseases and variants are constantly emerging. Healthcare professionals need to continually update their knowledge base on the latest dermoscopic diagnostic techniques and research findings by attending seminars and training courses.

Conclusion
The key to dermatoscopy is the use of optical magnification and polarization modes to help the physician better visualize the lesions, and IBOOLO has a wide range of dermatoscopes to meet your different needs. For more information about IBOOLO dermatoscopes, please visit the product section of the website. Dermoscopy is valuable in diagnosing skin tumors, evaluating skin inflammation, detecting hair diseases, and identifying parasitic infections. It can help doctors determine the nature of skin lesions, such as benign or malignant, and provide guidance for surgical removal. IBOOLO dermatoscope can definitely provide to be your most reliable seeing instrument in the daily visits of dermatologists.
The Standard Dermoscopy Procedure: A Clinical Guide to Skin Cancer Examination
The transition from a basic visual skin check to a professional skin cancer dermoscopy screening requires a commitment to clinical precision and a standardized dermoscopy procedure. By eliminating surface glare and magnifying micro-anatomical structures, a dermoscopy examination significantly reduces the rate of misdiagnosis in both melanocytic and non-melanocytic skin cancers. This guide outlines the evidence-based steps for performing a high-quality examination using advanced optical systems.
Phase 1: Pre-Examination Preparation
The integrity of a dermoscopy procedure begins before the lens ever touches the skin. Proper preparation ensures that subtle clinical signs are not obscured by external factors.
- Patient Consent and History: Document any history of rapid lesion growth, bleeding, or family history of melanoma.
- Skin Site Preparation: The area must be cleansed of cosmetics, sunscreens, or heavy topical ointments. For high-reflectivity lesions, ensuring the skin is dry is vital for non-contact polarized imaging.
- Equipment Check: Verify that the IBOOLO dermatoscope is clean and that the battery level is sufficient to maintain consistent LED intensity throughout the examination.
Phase 2: Executing the Dermoscopy Examination
During the dermoscopy examination, the clinician must decide between two primary modes of visualization, depending on the lesion's characteristics and location.
1. Immersion Dermoscopy (Non-Polarized)
This traditional dermoscopy procedure involves applying a liquid medium (link-oil, alcohol, or ultrasound gel) to the skin. This matches the refractive index of the stratum corneum, allowing light to penetrate directly. This mode is excellent for visualizing superficial structures like milia-like cysts and comedo-like openings, providing a sharp view of the skin's surface texture.
2. Cross-Polarized Dermoscopy (Non-Contact)
Utilizing the cross-polarization feature of the IBOOLO DE-4100 Pro, clinicians can visualize deeper vascular patterns and crystalline structures (shiny white streaks) without direct skin contact. This is often the preferred method for skin cancer dermoscopy as it avoids the compression of small blood vessels, which is critical for identifying the arborizing vessels of basal cell carcinoma.
Phase 3: Systematic Pattern Analysis and Triage
A professional dermoscopy examination is incomplete without a structured analytical framework. Clinicians typically apply a validated algorithm to determine the risk level of the lesion:
- The 3-Point Checklist: Assessing for asymmetry, atypical network, and blue-white structures.
- Vascular Triage: Identifying the morphology (dotted, linear, or polymorphic) and distribution of the blood vessels.
- Structural Mapping: Evaluating the presence of pathognomonic signs such as leaf-like areas, spoke-wheel structures, or regression signs.
Procedural Workflow: Manual vs. Digital Documentation
| Procedural Step | Manual Handheld Procedure | Digital (Smartphone-Link) Workflow |
|---|---|---|
| Initial Assessment | Real-time ocular evaluation. | On-screen high-definition viewing. |
| Record Keeping | Clinical drawing or text notes. | High-resolution 4K image storage. |
| Longitudinal Tracking | Difficult to assess subtle changes. | Sequential Digital Dermoscopy (SDDI). |
| Teledermatology | Not applicable. | Instant sharing for secondary opinions. |
Optimizing Results with IBOOLO Clinical Solutions
The success of any dermoscopy examination is intrinsically linked to the optical performance of the hardware. IBOOLO precision instruments are designed to enhance the dermoscopy procedure through:
- Advanced Lens Coatings: Premium Japanese glass lenses minimize chromatic aberration, ensuring accurate color reproduction of "milky-red" areas or blue-gray nests.
- Multi-Mode Illumination: IBOOLO devices allow for instant toggling between polarized and non-polarized light, enabling a comprehensive dual-mode assessment in seconds.
- Universal Integration: Our magnetic smartphone adapters transform any handheld device into a powerful digital imaging system, supporting the modern requirement for documented patient care.
Frequently Asked Questions
What is the most important step in a dermoscopy procedure?
The most critical step is achieving optimal focus and lighting. Without edge-to-edge clarity, subtle indicators of early malignancy, such as tiny blue-gray globules or fine vessels, may be missed.
Is a gel interface required for all examinations?
No. While a gel is necessary for non-polarized immersion dermoscopy, many clinicians now prefer polarized light for skin cancer dermoscopy because it is faster and does not require skin contact.
Can a dermoscopy examination differentiate all skin cancers?
While it significantly increases accuracy, dermoscopy is a triage tool. Any lesion that remains suspicious after a thorough dermoscopy procedure should be prioritized for a histopathological biopsy.






















