DE-400 Dermatoscope – IBOOLO
The Dermascope: A Powerful Ally for Dermatologists
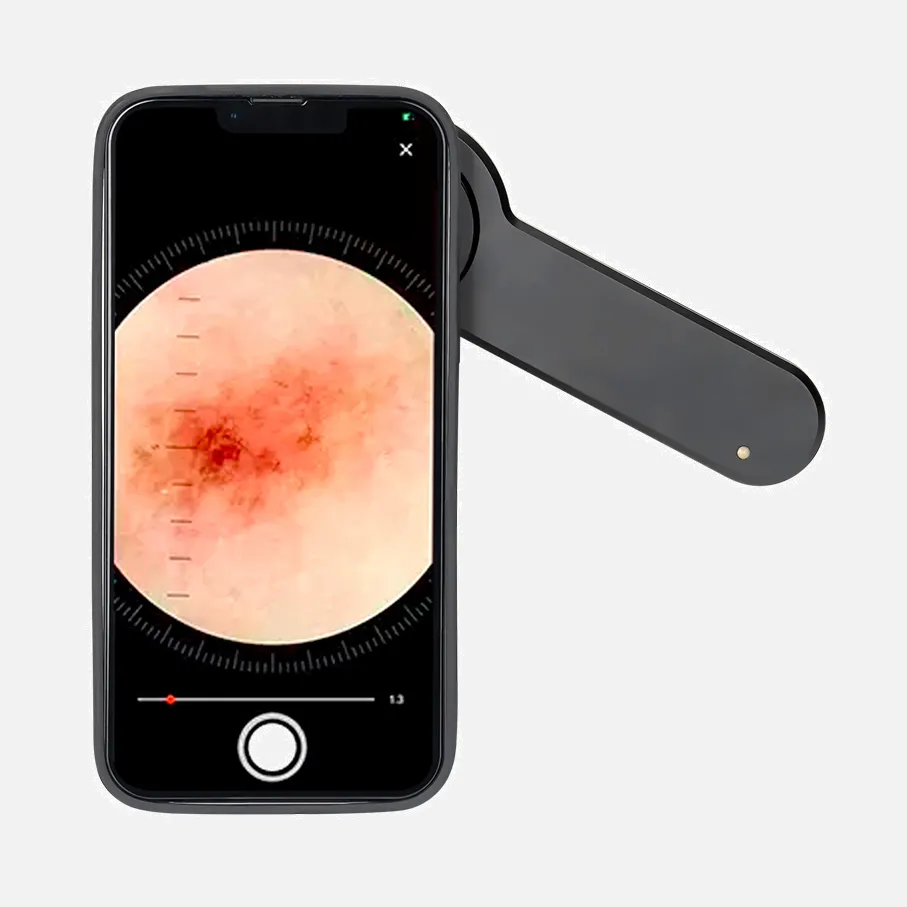
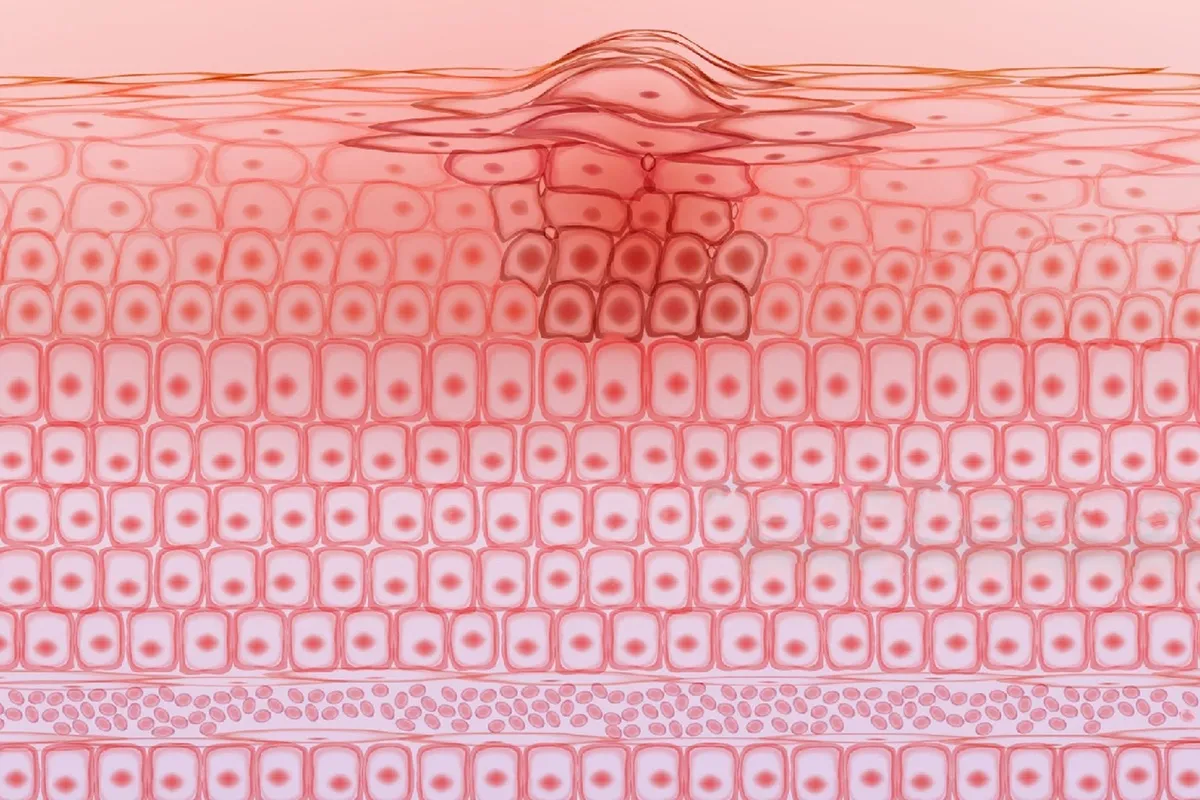
The dermascope, also known as a dermoscope or chemiluminescence microscope, is a non-invasive diagnostic tool that allows doctors to visualize microscopic structures beneath the skin's surface. With advancements in medical technology, the dermascope has become an indispensable tool in modern dermatology, playing a pivotal role in the early detection of skin cancer and diagnosis of various skin lesions.
How Dermoscopic Work
Dermascopes utilize a transparent compression plate and an integrated light source to magnify the skin's surface by approximately 10 to 200 times. This magnification capability enables physicians to observe details beneath the skin's outer layer, such as vascular patterns, pigment networks, and the microscopic structures of skin lesions. Dermascope plays a crucial role in medical diagnosis, particularly in the field of dermatology, serving several key purposes: early lesion detection, improved diagnostic accuracy, lesion monitoring, reducing unnecessary biopsies, education and training, patient self-examination, research tool application, cosmetic dermatology, assisting surgical planning, and increasing patient awareness.
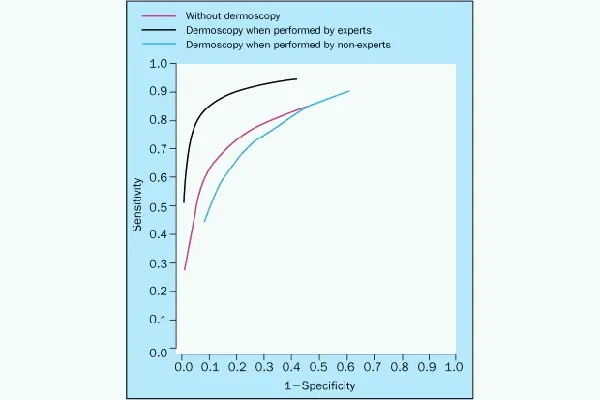
Skin Cancer Detection
Skin cancer is among the most common types of cancer, and early detection is critical for improving treatment success rates. The principles behind using a dermascope for skin cancer detection include: enhancing contrast, observing microscopic structures, identifying characteristic patterns, analyzing vascular patterns, recognizing color changes, assessing borders, evaluating skin translucency, dynamic monitoring, and aiding diagnosis. The use of dermascopes has significantly improved the accuracy of early detection of melanoma and other skin cancers. By identifying irregular pigment patterns, asymmetric borders, and color variations, doctors can more quickly identify suspicious lesions.
Clinical Applications
Dermascope has extensive applications in clinical practice as a non-invasive diagnostic tool that assists doctors in observing microscopic structures beneath the skin's surface, thereby improving the accuracy of diagnosing various skin lesions. The main clinical applications of dermascopes include: diagnosing pigmented tumors, non-pigmented skin lesions, erythematous papulosquamous skin diseases, hair and nail disorders, infectious diseases, aiding diagnosis and differential diagnosis, digital monitoring, guiding biopsies and excisions, increasing diagnostic accuracy, education and training, and patient self-examination. In clinical practice, dermascopes are used not only for diagnosis but also for monitoring treatment efficacy and lesion progression, helping doctors determine if a biopsy is needed and plan the boundaries for surgical excision.
Interpreting Dermatoscopic Images
Interpreting dermatoscopic images is a professional skill that requires training and practice. By identifying specific dermatoscopic features, such as morphological features, vascular signs, pattern analysis, characteristics of specific lesions, dynamic monitoring, quantitative image analysis techniques, remote Dermascope, comprehensive assessment, color features, globular and linear structures, doctors can differentiate between benign and malignant lesions.
Comparison with Other Diagnostic Methods
As a non-invasive skin diagnostic tool, dermascopes possess unique advantages and limitations compared to other diagnostic methods. Here is a comparison of dermascopes with other common skin diagnostic methods:
1. Compared to visual examination: dermascopes can magnify the skin's surface, revealing microscopic structures and pigment patterns that are difficult to detect with the naked eye, significantly improving diagnostic accuracy for skin lesions like melanoma.
2. Compared to biopsies: Biopsies are invasive procedures that involve taking skin tissue samples for pathological analysis to confirm a diagnosis. dermascopes are non-invasive and can reduce patient discomfort and risk.
3. Compared to Wood's lamp: Wood's lamps use ultraviolet light to illuminate the skin and observe the fluorescence of lesions, particularly useful for diagnosing certain fungal infections and depigmenting conditions like vitiligo. dermascopes provide more detailed information about the skin's surface and shallow structures and apply to a wider range of skin lesion diagnoses.
4. Compared to skin confocal microscopy: Confocal laser scanning microscopy can provide high-resolution, real-time images of living skin cells and tissue structures. However, dermascopes focus more on macroscopic observations of the epidermis and superficial dermis, which is particularly useful for diagnosing pigmented lesions.
5. Compared to skin ultrasound: Skin ultrasound uses high-frequency sound waves to examine deeper skin structures, helping diagnose subcutaneous lesions like cysts and tumors. In contrast, dermascopes focus more on epidermal pigment changes and superficial vascular patterns, which are crucial for the early diagnosis of skin cancer.
6. Compared to histopathology: Histopathology involves analyzing skin tissue samples obtained through biopsy, which is the gold standard for diagnosis. dermascopes are an auxiliary diagnostic tool that can improve the accuracy of clinical diagnoses but cannot replace pathological diagnosis.
History And Future of Dermascopes
The history of dermascopes can be traced back to the 19th century when their designs were relatively simple. Over time, dermascope technology has undergone significant advancements, with modern dermascopes featuring advanced optical systems and digital imaging capabilities. Although dermascopes are valuable tools, they have some limitations. For instance, their accuracy may be influenced by the operator's experience, and observing certain skin types or lesion locations may be more challenging. Future dermascope technology may integrate artificial intelligence and machine learning algorithms to improve diagnostic accuracy and efficiency. Additionally, as mobile device technology advances, portable dermascopes could become part of personal health management.
Selecting And Buying Dermascope Devices
Need analysis: Determine how you will use the dermascope, whether for personal daily skin checks or professional medical purposes. Consider the skin areas you need to observe and whether you need a portable device or a fixed workstation-style device.
Magnification and resolution: Choose the appropriate magnification and resolution based on the type and size of the skin lesions you will be observing. Ensure the selected device can provide clear images for accurate diagnosis.
Imaging technology: Understand different types of imaging technologies, such as polarized light, immersion contact, or non-contact. Choose the imaging technology that best suits your needs for observing different layers of the skin.
Additional features: Consider whether you need additional features like built-in light sources, digital image capture, image storage, and analysis software. Some advanced devices may also have the ability to connect with smartphones or computers for image sharing and remote diagnosis.
Portability: If you need to use the dermascope in different locations, a portable device may be more suitable. portable dermascopes are typically smaller and easier to carry and store.
Brand and price: Consider the brand and price of the device, choosing products with good value for money. Read user reviews and professional evaluations to understand the reputation and performance of different brands.
After-sales service: Learn about the manufacturer's warranty policies and after-sales service. Choose brands that offer good customer support and repair services.
Training and education: If you are a new user of dermascopes, choosing a brand that provides training and educational resources may be more important. Some manufacturers may offer online tutorials, seminars, or certification courses.
Regulatory compliance: Ensure the selected device complies with local medical device regulations and standards.
Trial and demonstration: If possible, try out the device or watch a demonstration before purchasing. This will help you understand the device's user interface and actual imaging performance.
The dermascope is a revolutionary tool that has greatly enhanced dermatologists' ability to diagnose skin lesions. It can help doctors detect skin cancer early, improving treatment success rates. As technology continues to advance and education becomes more widespread, dermascopes will play an increasingly important role in future dermatological practices. Regular dermatoscopic examinations and professional image interpretation can more effectively monitor and manage skin health.
People May Ask
Your skin will first be treated by the physician with an ultrasonic gel or oil (like mineral oil). The dermatoscope can capture clearer images when it is coated with gel or oil. After applying the gel or oil, the medical professional will gently insert the dermatoscope into your skin.
A novel and intriguing morphological aspect of pigmented skin lesions has been revealed by the clinical application of dermoscopy. Through the visualization of morphological traits invisible to the unaided eye, dermoscopy is a non-invasive diagnostic method that connects clinical dermatology and dermatopathology.
While Dermlite DL II only has cross-polarized mode, Heine Delta 20 only has non-polarized mode, which necessitates a contact fluid. The non-polarized dermatoscope aids in identifying the skin's surface structures, whereas the polarized dermatoscope permits more profound viewing.
A handheld device known as a dermatoscope is used to perform dermoscopy. Subsurface skin structures in the epidermis, papillary dermis, and dermoepidermal junction-structures that are often invisible to the unaided eye-can be seen thanks to this method [2-4].
A doctor or individual can inspect and diagnose skin lesions and disorders, including melanoma, using a dermatoscope, a hand-held visual assistance equipment. Examining the nails, hair, and scalp can also be facilitated by it. A dermatologist's practice typically has a dermatoscope.
On the mole that bothers you, apply one drop of oil. Directly touch the skin with the dermatoscope, press down gently, and use your smartphone to take a picture. Touching the screen's center may be necessary to concentrate the mole's image. Take and preserve clear dermoscopic pictures.
On dermoscopy, reticle ridges that are longer and broader due to greater junctional nests of melanocytes will show as wider and darker lines. The atypical network is frequently observed in dysplastic nevi and melanoma.
On the other hand, early diagnosis in cases in their early stages provides a chance to increase survival rates by timely surgery. There's no formal guidance regarding when to start therapy, even though many doctors operate on melanoma patients three to four weeks after diagnosis.
Clinically diagnosing nodular melanoma can be challenging. If melanoma characteristics are not observed around the lesion, it may potentially go undetected during a dermoscopy. The lesion might consist of just two or three colors, dispersed pretty symmetrically. Nodular melanoma accounts for 60% of amelanotic cases.
Even with dermoscopy, many lesions-particularly early melanomas-may be difficult to diagnose because they lack distinct dermoscopic characteristics.
Dermascope Products

Portable Ear Light and Exam Kit for Home and Professional Use - Cynamed Mini Otoscope - 3X Magnifying Fiber Optic Scope with Extra Tips, Bulb, and Carrying Case - Pocket Diagnostic Tools (Black)
Disposable ear specula for adults and older children, Treela 200 PCS Otoscope Cover Plastic Otoscope Specula Tips (4.25 mm, 200 Pieces)
KMDES Wireless Digital Microscope: Handheld USB HD Inspection Camera with 50X–1000X Magnification, Adjustable 8 LED Lights, and Stand Upgrade that Prevents Shake for PC Phone Compatibility. Available in White

A veterinary otoscope Pet Otoscope, Canine Otoscope, Ophthalmoscope Set, Ear Exam, Professional Diagnostic, Vet Otoscope Set, Otoscope for Dogs, Earache, Ear Canal Exam, Eardrum Exam, Premium
Handheld Microscope for Children and Students, HUTACT Pocket Microscope for Kids, 60X-135X Mini Portable Microscope with 5 Microscope Slides

The M82ES-SC100-LP100 OMAX 40X-2000X LED Binocular Compound Lab Microscope comes with a double layer mechanical stage, blank slides, cover slips, and lens cleaning paper.

Hair Analyzer for Skin Diagnosis, 12 inch Skin Scalp Detector, Multifunctional Hair Follicle Skin Analyzer Machine, Easy to Use, 110240V Rechargeable US

Adult 2000x Digital Microscope with 3 Lenses and 2160P UHD Video Recording, 7-Inch LCD Soldering Microscope, Coin Microscope, Biological Microscope Kit, Windows Compatible: Andonstar AD246S-M

Carson Pocket Micro Aspheric Lens System 20x-60x LED Illuminated Zoom Field Microscope (MM-450), Blue

MEDCASE Radiance Otoscope with Light German Fiber Optic - LED Lighted Ear Scope with Speculum for Ear Assessment and Diagnosis - Perfect for Both Home and Professional Use - Available in Purple Color
Hot Products
News & Blog
Top Reviews
I have three years old with this clip. It is incredible. Any type of stethoscope you use will fit into it with ease. I own a Welch Alyn with replaceable heads. I have no issue carrying either and I frequently swap between adult and pediatric diaphragms. I anticipate using this for many years to come because of the excellent craftsmanship. Pros: -The greatest benefit of this equipment is the shoulder relaxation it provides. The stethescope may start to weigh heavily on your shoulders after 12 to 30 hours. This is wonderful to have sitting on my hips. - It is simple to retrieve the stethescope. Just pull the strap back, allowing it to drop into your other hand. It only takes a few seconds, and you are set to go. "-The stethoscope that was hanging from the neck was no longer able to obstruct or strike patients in the face. -A lifetime warranty, I believe. Drawbacks: -The stethescope produces a loop by your side that may get entangled in objects. It takes roughly 5 seconds to replace the stethescope in the batclip, which is a little longer than it takes to wear it around your neck.
How does going to a code feel when your steth is around your neck? Akin to attempting to revive a bowling ball while positioned like a bowling pin. You don't have an issue if it's in your jacket, but it may fall out at any minute (eek). Then, when you put your head to the patient's chest to listen to their heart, they say something like, "Hey, you're not a doctor," and things get messy. So, explain why you think you should carry a clip with your stethoscope attached. much like BATMAN. Think about this. With all the confidence you have from not getting slapped in the face with your own tools and always knowing where they are, you walk into that code with your neck unencumbered and, with one great thrust, you've cleared out that pesky triple coronary blockage and your patient now has ROSC. You may even pull it out, play it, and force it back to the video, but proceed with caution—the nurses might pass out from the sight of your incredible CPR skills. It has come to my attention that when I sit in an auditorium chair, the screen
I work as a doctor, and I frequently get headaches. I detest wearing anything around my neck because even a small weight can cause excruciating tension headaches in me. A white coat or even a stethoscope around my neck bothers me. I attempted to swallow it for a few years before putting my stethoscope in my hand or slung over one shoulder—both awful choices. I attempted to use the inexpensive hip holster I had received for free from somewhere, but the hard plastic form makes it impossible for it to actually clip onto your waistband, and getting your stethoscope in and out of those things is surprisingly difficult. Insert the Batclip here. I became aware of them when one day one of my coworkers walked confidently into work wearing one on his hip. I was instantly sold because it had a polished, useful, and cozy appearance. That day, I bought one, and I was thrilled to find that it is just as wonderful as I had anticipated. It is simple to use, the clip fits well on scrubs or slacks with or without a belt, it