DE-400 Dermatoscope – IBOOLO
Dermoscopy Basal Cell Carcinoma
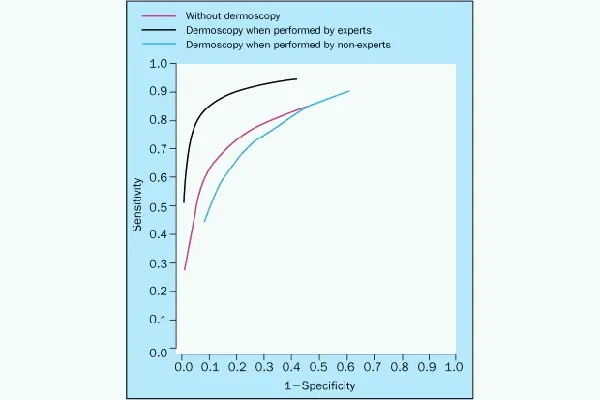
Dermoscopy is a non-invasive technique that can help diagnose basal cell carcinoma (BCC) early. Dermoscopy can accurately diagnose BCC up to 95–99% of the time.
Dermoscopic features of superficial BCC include:
- Ulceration and adherent fiber
- Leaf-like areas, which are brown to grey-blue discrete bulbous blobs that often form a pattern shaped like a leaf
Comma vessels
- Hemorrhage
- Small ulcerations
- Hypopigmented areas
- Telangiectasias
- Blue-gray ovoid nests
- Asymmetrical arborising vessels
Dermoscopy can also help identify BCC by the presence of typical vascular structures, pigmented structures, and ulceration, and the absence of specific melanocytic structures.
BCC is one of the most common cancers in white people, and its worldwide incidence is continuously increasing. Lesions from BCC usually have one of the following characteristics:
- A shiny, skin-colored bump that's translucent
- A bump that can look pearly white or pink on white skin
- A bump that often looks brown or glossy black on brown and Black skin
How Does Dermoscopy Basal Cell Carcinoma?
Dermoscopy is a non-invasive technique that can help diagnose basal cell carcinoma (BCC) early. It works by transilluminating a lesion, which allows it to be studied at high magnification to see subtle features.
Dermoscopic criteria associated with BCCs include:
- Absence of a pigment network
- Arborizing vessels
- Large blue-gray ovoid nests
- Multiple blue-gray globules
- Leaf-like areas
- Spoke wheel areas
- Ulceration
Other dermoscopic features of BCC include:
- Unfocused peripheral arborizing vessels
- Keratin masses
- Superficial scales
- Ulceration or blood crusts
- White structures
- Blue-gray blotches
BCC's Dermoscopic diagnostic accuracy is 95%–99%. However, a diagnosis of BCC should not be based on a single feature but on a set of dermoscopic features in combination with the clinical context.
Experienced dermoscopists can often diagnose superficial BCCs by their typical bluish-pink color.
People May Ask
Asymmetric pigmented follicular openings, dark rhomboidal structures, slate gray dots, and slate gray globules are the four criteria that together have produced an 89% and 96% diagnostic sensitivity and specificity.
The Use of Dermoscopy in BCC ManagementFor the assessment of residual tumor in BCC patients, dermoscopic examination following nonablative treatment has also shown promise. Remaining dermoscopic characteristics such as arborizing telangiectasias, ulceration, and pigmented formations are good markers of tumor persistence.
In the absence of therapy, a basal cell carcinoma has the potential to slowly spread throughout a significant portion of your body's skin. Furthermore, ulceration and long-term harm to the skin and adjacent tissues are potential side effects of basal cell carcinoma.
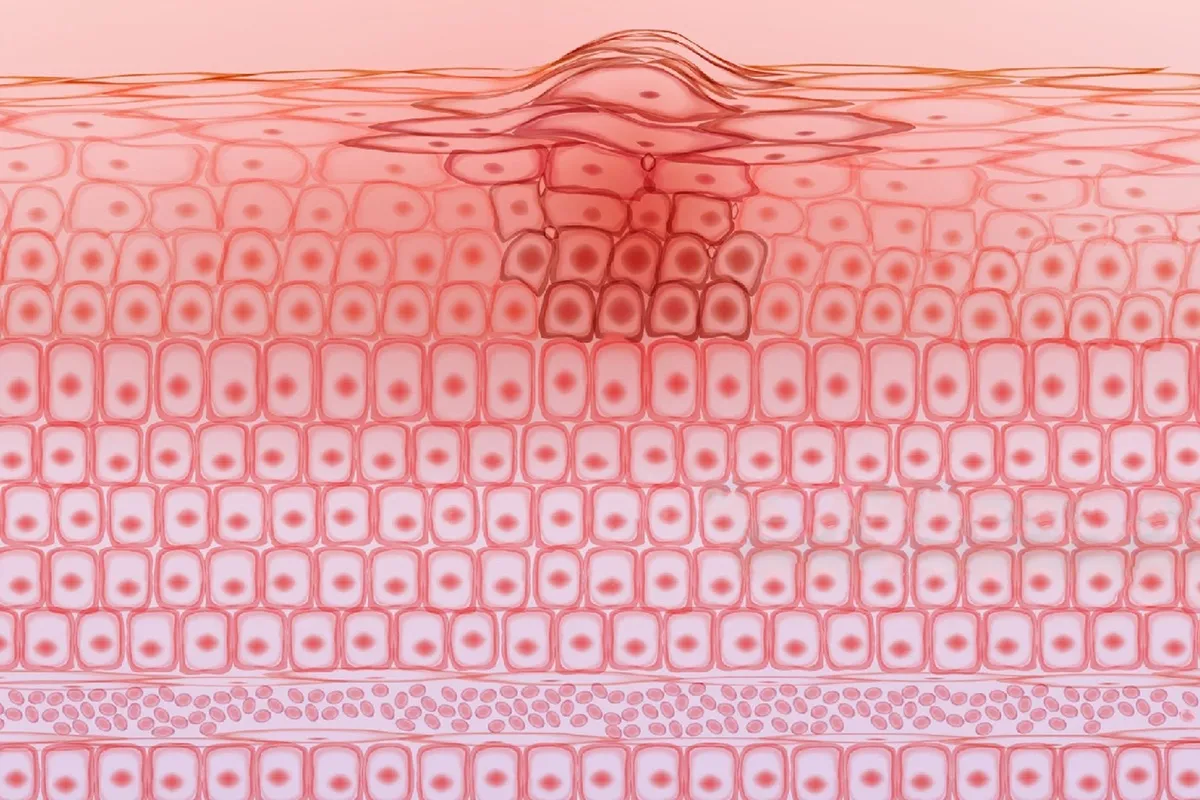
relative mass confinement.There is varying degrees of epidermal or follicular attachment.Large nuclear palisade-surrounded basaloid lobules.Because of the overproduction of mucin, loculules may be solid or exhibit central cyst development.Scleromyxoid stroma.A cleft forms in the stroma between the tumor lobules.Instead,Additional things...
a translucent, skin-colored pimple that is glossy and partially transparent. When compared to pink skin, the bump can appear pearly white. The bump frequently appears brown or glossy black on skin that is brown or black.
How does a BCC look? Open sores, red spots, pink growths, shiny bumps, scars, or growths with slightly elevated, rolling edges and/or a center indentation are some of the appearances of BCCs. BCCs have the potential to leak, crust, itch, or bleed. The lesions usually appear on body parts that are exposed to the sun.
It is known as a skin biopsy and can be completed in the course of an office visit. A dermatologist can easily, swiftly, and securely execute this straightforward operation. The only way to be positive for any kind of skin cancer is to undergo a skin biopsy.
Common dermoscopic characteristics of carcinomas with cutaneous squamous cell carcinoma are:Instead,White circles.
White patches devoid of structure.Vessels with loops.Keratin in the center.When a tumor is poorly differentiated or growing quickly, the background may be pink or red.
Furthermore, comma vessels, hemorrhage, minor ulcerations, hypopigmented regions, telangiectasias, and blue-gray ovoid nests are characteristics of superficial BCCs, whereas arborizing vessels are also characteristic of nodular BCCs.
With their characteristic bluish-pink color, asymmetric arborizing vasculature, and focal ulceration, superficial basal cell carcinomas are often diagnosed by skilled dermoscopists. White regions of regression and little scaling could also exist.
Dermoscopy Basal Cell Carcinoma Products

January 1, 2017: The Natural and Quick Cure for Staple Bound Basal Cell Carcinoma

The 30-Day Raw Vegan Plant-Based Detoxification & Regeneration Journal & Tracker: Healing Nevoid Basal Cell Carcinoma Syndrome A Reversing Conditions Journal and Tracker. Journal 2 - February 28, 2020 - Paperback

A Clear Guide to Medical Conditions: Diagnosis and Treatment of Basal Cell Carcinoma Kindle攵子书

Sunspot ES, Natural Exfoliating Gel with Aloe Vera and Tea Tree Oil for Skin Renewal Ingredients by Lane Innovations (0.5 oz, 2 pack)

First Edition of Dermoscopy in Darker Skin, Kindle Edition

Ebook Enhanced Segmentation-Based Method Utilizing PSO and K-MEANS Algorithm for Basal Cell Carcinoma Identification from Skin Lesions

Pink-Think-Blink, First Edition, Kindle Edition: Dermatoscopy of Non-Pigmented Skin Tumors

Kindle Edition of Practical Dermoscopy

Aloe vera and tea tree oil are among the skin-rejuvenating ingredients in Lane Labs SunSpot ES, a natural exfoliating gel (0.5 ounce).
Actinic Keratosis: Learn how to reduce your risk of skin cancer and avoid recurrence to replace your anxiety and uncertainty. Kindle攵子书
Related Products
Hot Products
News & Blog
Top Reviews
My second tube of Sunspot Es is this one. Since my first tube's results were so good, I bought a second one after a friend convinced me not to use it for her issue. Regrettably, the FDA is refusing to let the firm disclose that its true benefit is treating minor skin malignancies. I mean business. My personal experience was with a basal cell carcinoma on my ankle that the doctor wanted to remove. Despite my hesitation, I tried this Sunspot. Es product. Over the course of two weeks, it performed flawlessly except from occasional stinging and itching. On his cheek, my spouse had a large area of keratoses. It looked terrible, and it bled every now and again. Reluctantly, he gave the Sunspot Es a try, and was astonished to discover how powerful it was. The spot took around a month to vanish since he neglected to apply a bandage. When applied correctly, it is an excellent product for treating kerotases, squamous cell, or basal cell carcinomas. I was aware that removing a malignancy using traditional techniques results in significant harm or destruction of the surrounding tissue, which
I was pleasantly surprised to find this book contained much more than the dull, elementary content I had assumed based on its cover. This book has an easy-to-read, pleasant, and sympathetic tone, but its substance is jam-packed with reliable scientific data and practical advice. Rather than merely wearing sunscreen and waiting for my next skin check, I'm so happy to finally have information that I can truly utilize to improve myself. I now have a ton of good actions that I can do to strengthen my immunity and maybe stop future eruptions, in addition to the therapeutic alternatives that this book explained. For the first time, I've been informed of alternatives to avoiding the sun, and I find that information to be really valuable.
Written for the BEST dermatoscopist, it's an excellent book with appropriate content, good photos, and helpful outlines. It's essential, in my opinion, for anybody with an interest in dermoscopy.