Case for iPhone – IBOOLO
People May Ask
A deficiency in serum vitamin B12 can be attributed to oral lichen planus. This vitamin is intricately connected with the optimal functioning of both the immune and neuropsychological systems, both of which are pivotal in the etiopathogenesis and potential malignant transformation of oral lichen planus. August 21, 2020.
This is a condition of an unknown origin, denoted as idiopathic, which triggers irritation within the skin layers. In the context of lichen planus, the immune system of the individual mistakenly targets certain bodily components rather than safeguarding the body against external threats such as bacteria or viruses.
The majority of skin lichen planus cases tend to resolve spontaneously within a timeframe of 6 to 9 months. Rarely does the rash persist for a duration exceeding 18 months. Nevertheless, it's noteworthy that oral lichen planus and its manifestation in the genital region may exhibit a more prolonged and persistent nature.
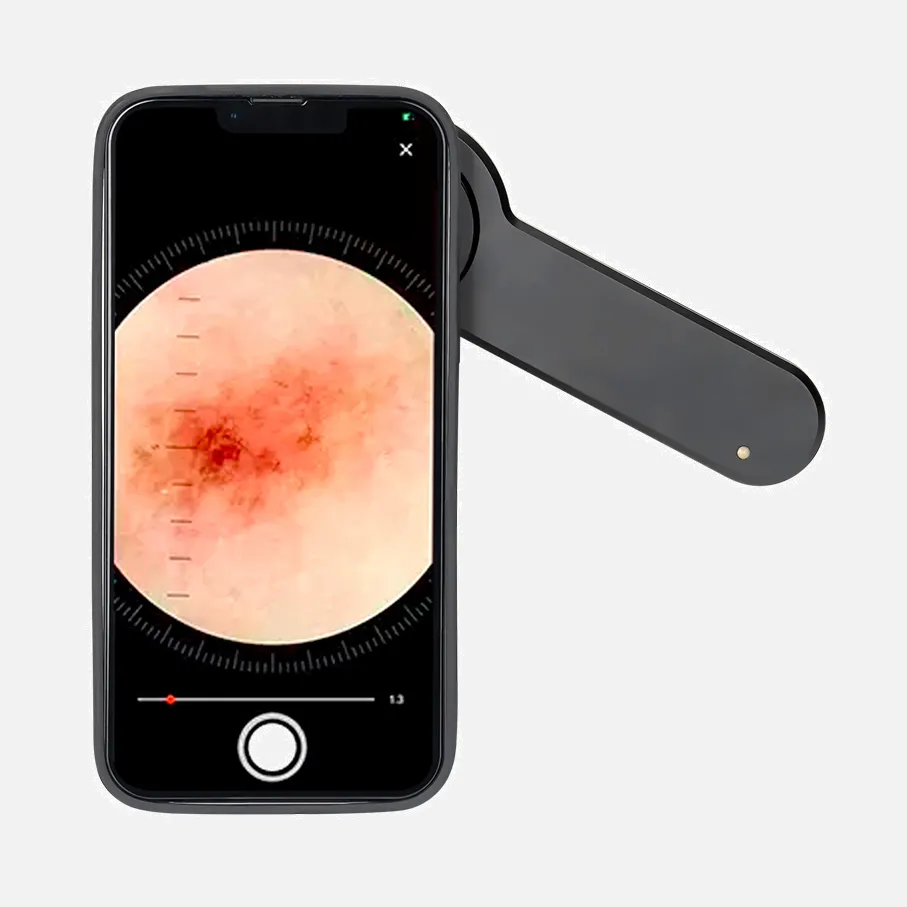
Addressing Benign Lichenoid Keratosis Condition
Application of Anti-Itch Cream -- to alleviate pruritus
Administration of Steroidal Medication, Both Orally and Topically -- to mitigate inflammatory symptoms
PUVA Therapy or Photochemotherapy Approach -- an innovative treatment modality employing ultraviolet radiation for sore management
Retinoid Acid Therapy -- a Vitamin A-based medication, frequently prescribed for acne vulgaris treatment
Date:
Drugs frequently implicated in eliciting a lichenoid drug-induced skin reaction encompass a variety of medications such as: Blood pressure medications like ACE inhibitors, beta-adrenergic blocking agents, nifedipine, and methyldopa. Additionally, diuretic agents such as hydrochlorothiazide, furosemide, and spironolactone are also known to precipitate this reaction. Moreover, non-steroidal anti-inflammatory drugs (NSAIDs) are among the medications that have been commonly reported to trigger such eruptions.
Occasionally, lichen planus can be erroneously identified as alternative dermatological conditions, including lichen sclerosus, which underscores the importance of consulting a skin expert (dermatologist) or a specialist in women's health (gynecologist) for accurate diagnosis.
Actinic keratosis represents an irregular proliferation of cells, stemming from prolonged exposure to the sun's harmful rays, he elaborates. While these lesions are non-malignant in nature, a minor percentage of them poses a risk of evolving into skin cancer.
The emergence of prototypical cutaneous lichenoid reactions as a result of medication intake can be attributed to various agents, including angiotensin-converting enzyme (ACE) inhibitors, antimalarial medications, beta-adrenergic blocking agents, gold compounds, lithium salts, mercury amalgam fillings, methyldopa, penicillamine derivatives, quinidine sulfate, sulfonylurea-based drugs for diabetes management, thiazide-class diuretics, inhibitors of tumor necrosis factor (TNF)-α, as well as tyrosine kinase inhibitors.
Categorization of oral lichen planus encompasses six distinct clinical manifestations: reticulate, plaque-mimicking, papular, atrophic/erosive, ulcerated, and bullous forms, as illustrated in Figure 1. These types predominantly impact the buccal mucosa, tongue, and gingival tissues.
In the context of lichenoid keratosis, the grayish specks encircling the follicular apertures are characteristically rough, uniform, and prevalent, whereas within lentigo maligna, these dots are markedly finer and concentrated in specific areas.