Case for iPhone – IBOOLO
People May Ask
Approximately 10 percent of actinic keratoses progress to malignancy, yet a substantial portion of squamous cell carcinomas (SCCs) initiate as AKs. Unfortunately, predicting which AKs will pose a serious threat remains elusive, necessitating vigilant monitoring and prompt intervention for any that arise as the sole means of ensuring safety.
The nature of melanoma is such that it often undergoes changes and enlargement over a period of time. It is therefore advisable for individuals who observe a growth resembling seborrheic keratosis but with alterations in its shape or hue to promptly seek medical advice. Additionally, it is essential to keep an eye out for the following indicators: Asymmetry: A mole or growth exhibiting a dissimilar appearance on one side could be a potential indicator of melanoma.
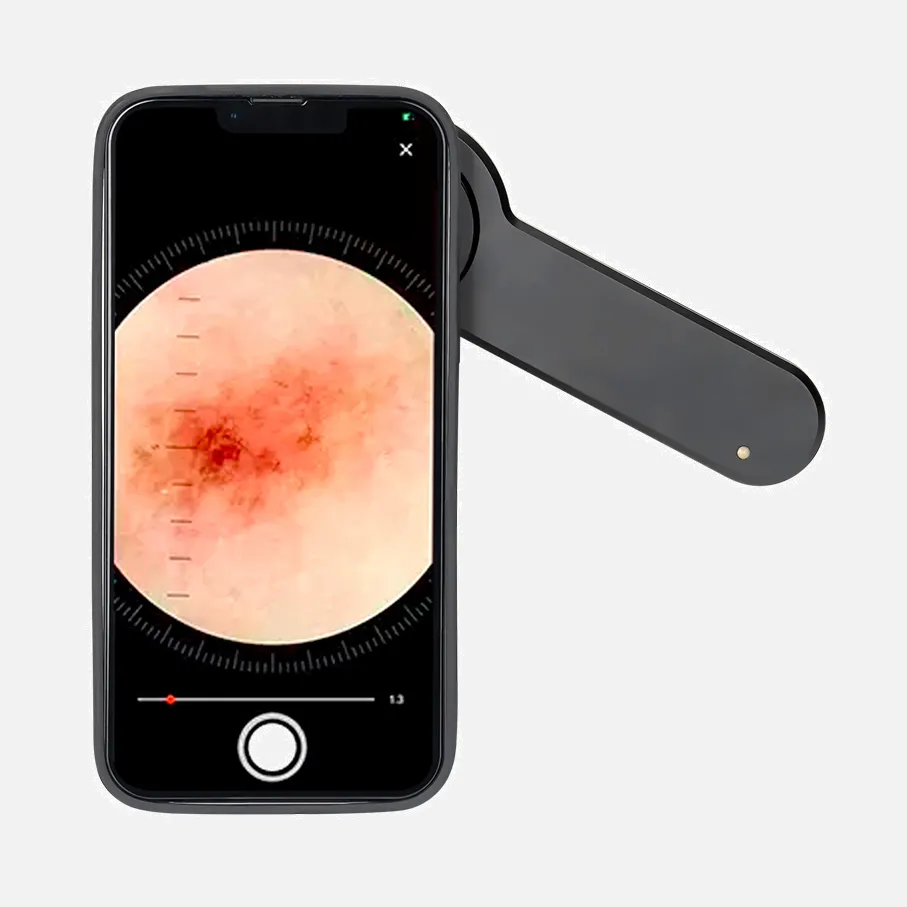
How do actinic keratosis and basal cell carcinoma present themselves visually?
Actinic keratosis manifestations are precancerous lesions. ...
These actinic keratosis lesions typically arise on the palms of the hands.
The color palette of pigmented basal cell carcinomas can vary based on an individual's skin tone.
Basal cell carcinoma commonly exhibits rounded contours and a central indentation.
28th of November, 2022
Premalignant skin conditions known as actinic keratoses have the potential to develop into squamous cell carcinoma. These lesions are typically observed in regions of the skin that have been exposed to the sun, especially among individuals with a background of prolonged sun exposure.
Adopting a healthy lifestyle and home-based treatments
Employ the use of lukewarm water and moderate bathing durations. Hot water and prolonged showers or baths tend to strip the skin of its natural oils. ...
Handle your skin with care. Steer clear of harsh, drying soaps. ...
Experiment with medicated lotions. ...
Keep your skin hydrated. ...
Utilize a humidifier. ...
Prevent irritation caused by tight-fitting clothing.
Actinic keratoses, alternatively referred to as senile keratoses or solar keratoses, are non-malignant neoplasms that arise within the epithelium and are frequently assessed by dermatologists. They are commonly linked to prolonged exposure to sunlight, and individuals suffering from actinic keratosis may exhibit irregular, reddened, scaly papules or plaques in sun-exposed areas of their bodies.
The mortality rate associated with cutaneous squamous cell carcinoma (cSCC) is notably elevated. It possesses distinctive attributes such as a diameter exceeding 2 cm, a depth greater than 5 mm, a propensity for high recurrence, perineural invasion, and the development of locoregional metastases. Among aggressive cSCC lesions, metastasis to the parotid gland is the most prevalent occurrence.
1. Consequences of Neglecting Actinic Keratoses? Neglecting actinic keratoses may lead to the development of skin cancer. Should you have experienced these skin lesions previously, only for them to disappear and later recur following repeated UV exposure, it is advisable to contact Worcester Dermatology in Worcester, MA to schedule a consultation.
Excision Method: In scenarios where an AK is exceptionally thick, this approach could be the optimal choice. In this procedure, your dermatologist employs a method called excision to carefully remove the AK from your skin. Optionally, following the excision, a technique called electrodesiccation may be utilized to heat the treated area, effectively eliminating any residual AK cells.
SCC manifests in the form of solid, flesh-hued keratotic papules, plaques, and smooth nodules. These lesions may be accompanied by a thick cutaneous horn and ulceration. Traits indicative of BCC include translucency, ulceration, the presence of telangiectasias, pigmentation, and a distinct rolled border. December 26th, 2017