DE-400 Dermatoscope – IBOOLO
Dermatoscopy: A Non-Invasive Skin Lesion Diagnostic Technique And Its Applications
What Is Dermatoscopy?
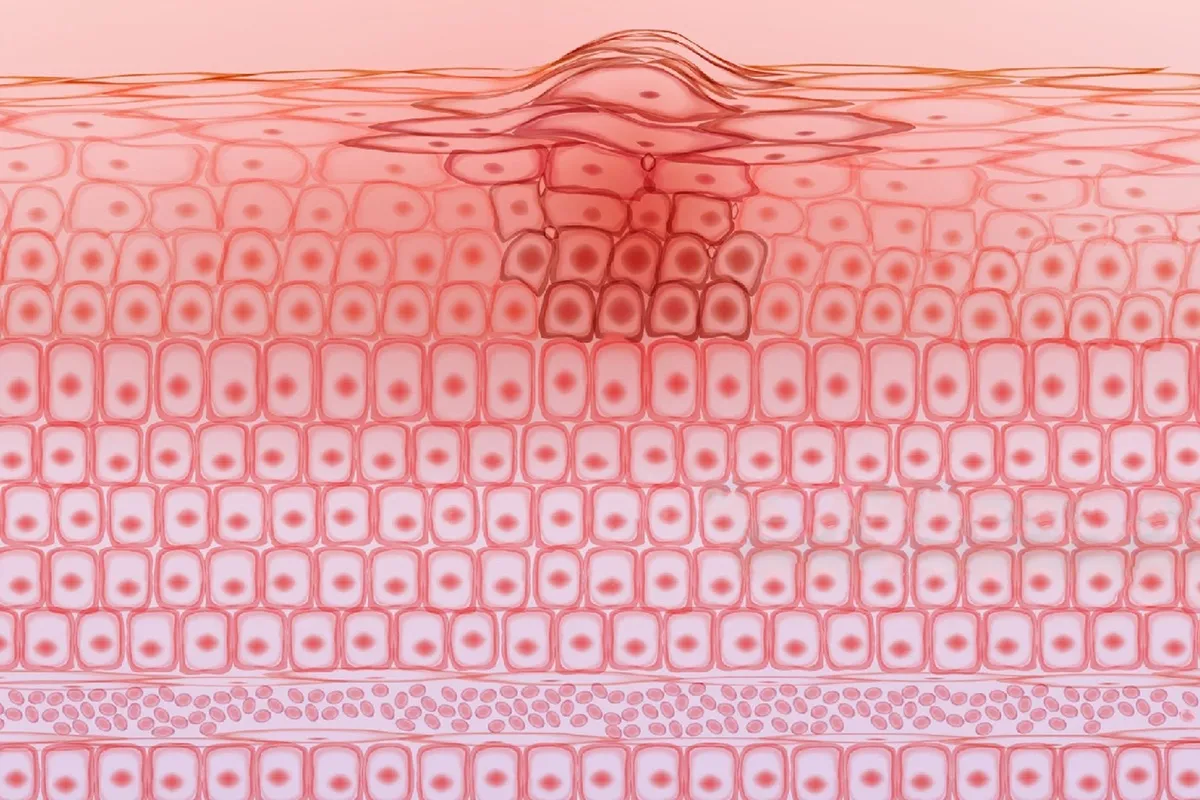
Dermatoscopy, is a noninvasive method that enables clinicians to evaluate fully - using a magnified oil immersion diascopy - numerous morphological features, not visible with the naked eye, which enhances the diagnosis of nearly all pigmented skin lesions.This examination can help doctors identify and differentiate skin lesions, such as moles, rashes, infections, and skin cancers. Its features include magnification capability, non-invasiveness, real-time imaging, image recording, and polarized light technology.
What Types of Dermatoscopy Are There?
Dermatoscopy is a non-invasive skin diagnostic technique that involves magnifying and illuminating the skin's surface to observe microscopic structures. The types include Handheld dermatoscopes - the most basic type, where doctors can directly observe skin lesions using a handheld device. polarized-light dermatoscopes use polarized light technology to reduce reflections from the skin's surface, making deeper structures more visible. Immersion dermatoscopes use oil or water mediums between the lens and skin to improve image clarity and resolution. Digital dermatoscopes incorporate digital imaging technology, allowing for capturing, storing, and analyzing high-resolution images, facilitating record-keeping and comparison of lesion changes. Reflectance confocal microscopes are an advanced dermatoscope technology that provides near-histological clarity with high-resolution images, enabling the observation of deeper skin structures. portable dermatoscopes are designed to be lightweight and convenient for use in different settings. Workstation dermatoscopes are typically connected to computer workstations and equipped with advanced image analysis and processing software. Dermatoscope imaging systems integrate diagnostic systems, photography techniques, and report printing, providing clear imaging and convenient operation.
Dermatoscopic Features of Pigmented Lesions
The dermatoscopic features of pigmented lesions can provide important diagnostic clues for doctors. Here are some common dermatoscopic features of pigmented lesions:
Pigment network is the most common Dermatoscopy presentation in melanocytic lesions. The network structure typically appears as brown streaks on a diffuse light brown background, covering most of a specific lesion. Globular structures are pigmented round or oval brown or grayish-black clumps of varying sizes, seen in Clark nevi and papillomatous intradermal nevi (Unna nevi). Ovoid blue-gray nests can be seen in pigmented basal cell carcinomas, appearing as well-defined, loosely connected oval nests or elongated areas, usually bluish-gray. Blue-gray globules are round or oval bluish-gray structures, which may appear brown or pinkish depending on the location of pigment within the tumor nests, often found in the dermal papillae or reticular dermis. Arborizing vessels are bright red vessels longer than 1mm, with a main trunk diameter ≥0.2mm and irregular branching patterns, typically representing the tumor's neovascular system.
Other features include radial streaming, which is radiating projections surrounding a central darker area (axis), with the projections appearing brown, blue, or gray, and the center appearing dark brown, blue, or black. The blue-white veil is a diffuse, confluent bluish-gray to bluish-white structure coexisting with different pigment networks, dots/globules, or streaks, almost exclusively seen in melanomas and Spitz/Reed nevi. pigment deposition refers to diffusely distributed deep brown to grayish-black areas, excluding structures with more refined features like pigment networks or vascular structures. Irregular pigment streaking, visible as irregular pigment extensions in malignant melanoma, is an important diagnostic clue. The blue-white veil exists in some pigmented BCCs, but its mere presence is not a key indicator for distinguishing pigmented BCCs from invasive melanomas in Chinese populations. These features are crucial for differentiating benign and malignant pigmented lesions, but the final diagnosis still requires considering clinical presentations, patient history, and histopathological examination when necessary.
Dermatoscopy Technique
Dermatoscopy is a non-invasive skin diagnostic method that involves magnifying and observing the skin's surface and subsurface structures using specific instruments, enabling more accurate identification and diagnosis of skin lesions. Dermatoscopy plays a vital role in the daily work of dermatologists, improving diagnostic accuracy and facilitating early detection of skin lesions. Here are some key points about the dermatoscopy technique:
- Definition: A dermatoscope (also known as a chemiluminescence microscope, incident light microscope, or skin surface microscope) is a non-invasive technique that allows observation of subsurface structures in the epidermis, dermal-epidermal junction, and papillary dermis.
- Classification: Dermatoscopes can be classified based on the imaging principle into immersion and polarized light types, or based on whether the lens contacts the skin into contact and non-contact types. There are also portable and workstation dermatoscopes, with the latter often connected to computers and pre-installed with various software applications.
- Applications: Dermatoscopes are primarily used to examine pigmented and non-pigmented skin lesions, helping doctors determine whether a skin biopsy, referral to a specialist, or continuous monitoring is needed.
- Process: The dermatoscopy process includes cleaning the skin, using the dermatoscope to observe or photograph the lesion area, and the doctor making a diagnosis based on the observed images.
- Advantages: As a non-invasive tool, dermatoscopy can significantly improve diagnostic accuracy for pigmented and non-pigmented lesions, reducing the need for blind surgical excisions or biopsies.
- Image quality control: To ensure the accuracy of dermatoscopy, image quality control is necessary, including appropriate lighting, resolution, and contrast.
- Diagnostic Terminology: Dermatoscopy diagnostic terminology includes metaphoric (analogical) terms and descriptive terms, with standardized terms aiding communication between doctors and diagnostic accuracy.
- Vascular signs: Vascular signs observed under the dermatoscope provide valuable auxiliary information for diagnosing inflammatory or tumor-related skin conditions.
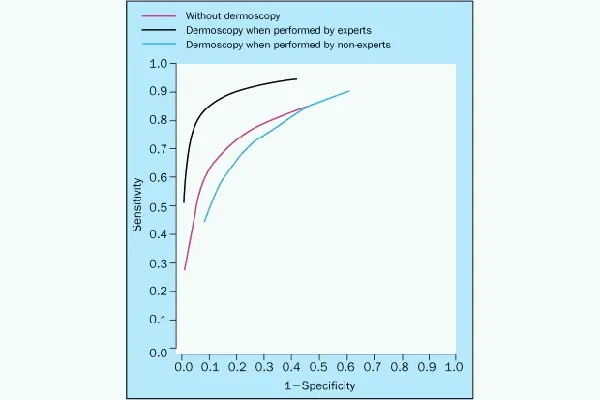
Effectiveness of Dermoscopy Examination
Non-invasive: Dermoscopy is a non-invasive technique, which means it does not cause any trauma or discomfort to the skin. As an auxiliary diagnostic tool, dermoscopy can significantly improve the diagnostic accuracy of pigmented and non-pigmented skin lesions. Moreover, dermoscopy examinations are quick and can provide immediate diagnostic results. Dermoscopy can also observe skin structures and changes that are not visible to the naked eye, such as those in the epidermis, dermal-epidermal junction, and upper dermis. The clinical application of dermoscopy reduces the probability of trauma caused by blind surgical excision or biopsy, avoiding unnecessary surgical excision. Dermoscopy examination can effectively guide the scope of surgical excision, postoperative follow-up, and the selection of appropriate physical therapy methods. Dermoscopy can not only dynamically monitor the disease course of skin lesions and suspicious lesions in high-risk populations but also, due to the high-definition imaging systems of modern dermoscopy equipment, facilitate detailed observation by doctors. Many dermoscopy devices are designed to be portable and easy to operate, with some even capable of connecting to smart devices for the convenience of doctors and patients. For pediatric patients, dermoscopy examination reduces the painful detection means of invasive examinations.
Dermatoscopy steps: preparation stage - the patient needs to clean the skin in the examination area. Examination process - the doctor carefully observes the suspected lesion area using the dermatoscope. Image recording - if necessary, the doctor will take pictures of the lesion area for analysis and recordkeeping. Diagnosis and recommendations - based on the observations, the doctor will provide a preliminary diagnosis and suggest further examinations or treatments.
Precautions for Dermoscopy Examination
Before undergoing a dermoscopy examination, patients should ensure that the skin in the area to be examined is clean and dry. Before the examination, cosmetics should be avoided on the lesion site, and no cosmetics or colored products should be applied, as this may affect the examination results. Since dermoscopy is non-traumatic, patients generally do not require special preoperative preparation. The examination is performed with the assistance of a dermoscope, and the doctor will provide necessary guidance to the patient before the operation. Additionally, skin disinfection or other procedures are usually completed by the doctor or nursing staff, and the patient does not need to handle them independently. During the examination, patients need not feel fear or anxiety about the process; they should simply maintain a relaxed state. After the examination, the doctor may provide further diagnostic or treatment recommendations based on the observed images. Patients who require regular monitoring of skin lesions should follow medical advice and undergo regular follow-up examinations.
People May Ask
Furthermore, malignant moles may cause no pain at all. However, in the event of a pigmented mole, this signifies melanoma. Certain moles that develop into cancer can also cause discomfort or peculiar sensitivity that is distinct from the surrounding skin.
Dermatologists, or medical professionals that specialize in treating skin conditions, treat the majority of basal and squamous cell malignancies as well as pre-cancers.
Skin cell alterations that increase the likelihood of cancer development are known as precancerous abnormalities of the skin. Currently, actinic keratosis is not cancer. However, it could progress to squamous cell carcinoma, a kind of non-melanoma skin cancer, if left untreated. Solar keratosis is another name for actinic keratosis.
The lesion or mole has been altering in size, shape, color, or appearance; it's also expanding into a previously normal-looking patch of skin. Additionally, melanoma may cause a mole or lesion's texture to change, becoming lumpy or hard.
Often, a mole that changes in size, shape, or color is the first indication of melanoma. There are two warning indicators of melanoma in this case: color fluctuations and an uneven border. Anywhere on your body, melanomas can form.
As 80% of lung nodules with a diameter of less than 2 cm are benign, the more benign a tumor appears on a radiograph, the smaller it appears. Though they are not the only indicators of benign tumors, smoothed radiopaque density with distinct edges characterize the majority of benign nodules.
When benign soft tissue tumors are located superficially, they rarely grow larger than two centimeters on average. However, deep tumors can grow up to several inches before being discovered, such as peripheral nerve tumors and angiomyolipoma.
Tumors may feel hard on the exterior, but studies have revealed that the individual cells within the tissue are not all the same rigidity; in fact, the tumors can vary in softness throughout.
What skin cancer appears likeChanging your mole or getting a mole that appears unique.Instead,dome-shaped development.Scaly patch.Instead,a sore that doesn't heal or one that heals then returns.Instead,beneath a nail, a brown or black streak.
A noninvasive in vivo method called dermoscopy is mainly employed to examine skin lesions [1]. Skin-surface microscopy, incident light microscopy, dermatoscopy, and epiluminescence microscopy are synonyms. A handheld device known as a dermatoscope is used to perform dermoscopy.
Dermatoscopy Products

Coins Electronic Magnifier Camera, 1000X Pocket Microscope for Kids and Adults, Use Indoors and Outdoors, Handheld Digital Microscope D-MS1 with 2 IPS Screen - Capture Photos and Videos - Download to PC & Mac

Clinical Cases in Dermatology: First Edition, First Edition, 2016 Kindle Edition of Clinical Cases in Skin Cancer Surgery and Treatment

UPDATED CLINICAL DERMATOLOGY HANDBOOK: A Brief, Accurate, and Thorough Overview and Bibliography of Skin Conditions Paperback - June 2, 2022

Supplementary Applications of Dermatoscopy, A Dermatologic Clinics Issue (The Clinics: Dermatology Book 36) Kindle攵子书

In the first edition of Dermatoscopy in Clinical Practice: Beyond Pigmented Lesions (Series in Dermatological Treatment), available on Kindle

Using dermatoscopy and fluorescent contact biomicroscopy in tandem to diagnose basal cell skin cancer 平装 – 2021年 6月 30日

Dermatoscopy and Skin Cancer: A Guide for Melanoma and Skin Cancer Hunters, First Edition
First Edition, 2018 of the Atlas of Pediatric Dermatoscopy

Dermatoscopy and Skin Cancer, Revised Edition: A Guide for Melanoma and Skin Cancer Investigators Revised Version

Chinese Traditional Medicine for Eczema Treatment