DE-400 Dermatoscope – IBOOLO
The Essential Guide to Medical Dermatoscope: Unlocking The Secrets of Skin Diagnostics
The History And Evolution of Medical Dermatoscopes
History:
The history of dermatoscopes can be traced back to the late 19th century when doctors began using magnifying glasses to observe skin lesions. In the early 20th century, dermatoscope technology advanced further, with doctors using magnifying glasses equipped with light sources to observe the skin more clearly. Over time, the design and functionality of Medical dermatoscopes continually improved, including the addition of polarized and cross-polarized light techniques, enabling doctors to more accurately diagnose skin lesions.
Develop:
In the 1950s, polarized light technology was introduced into medical dermatoscopes, which greatly enhanced doctors' ability to observe structures beneath the skin's surface. By the 1990s, with the development of digital technology, digital dermatoscopes emerged, allowing doctors to store and analyze images. At the beginning of the 21st century, automatic image analysis technology began to be integrated into medical dermatoscopes, improving the accuracy and efficiency of diagnosis.
What Is Dermoscopy in Medical Terms?
In medical terms, a dermoscope (also called a dermoscope) is a diagnostic tool used to magnify and illuminate the skin's surface and subcutaneous structures. It usually consists of a handheld device equipped with a magnifying glass and a light source, allowing doctors to observe small changes in the skin and deeper structures without the need for invasive examinations.
The Main Functions of Medical Dermatoscopes Include
Medical dermatoscopes can use the magnification function to allow doctors to see the tiny detailed lesions on the skin more clearly. There is a light source inside that can illuminate the skin and help doctors observe the underlying skin structure. polarized light technology reduces surface reflections, allowing deeper structures to be seen more clearly. Cross-polarized light technology further suppresses scattered light and enhances the concentration of light. Some dermatoscopes also feature digital cameras that capture and store images of the skin for recording and analysis.
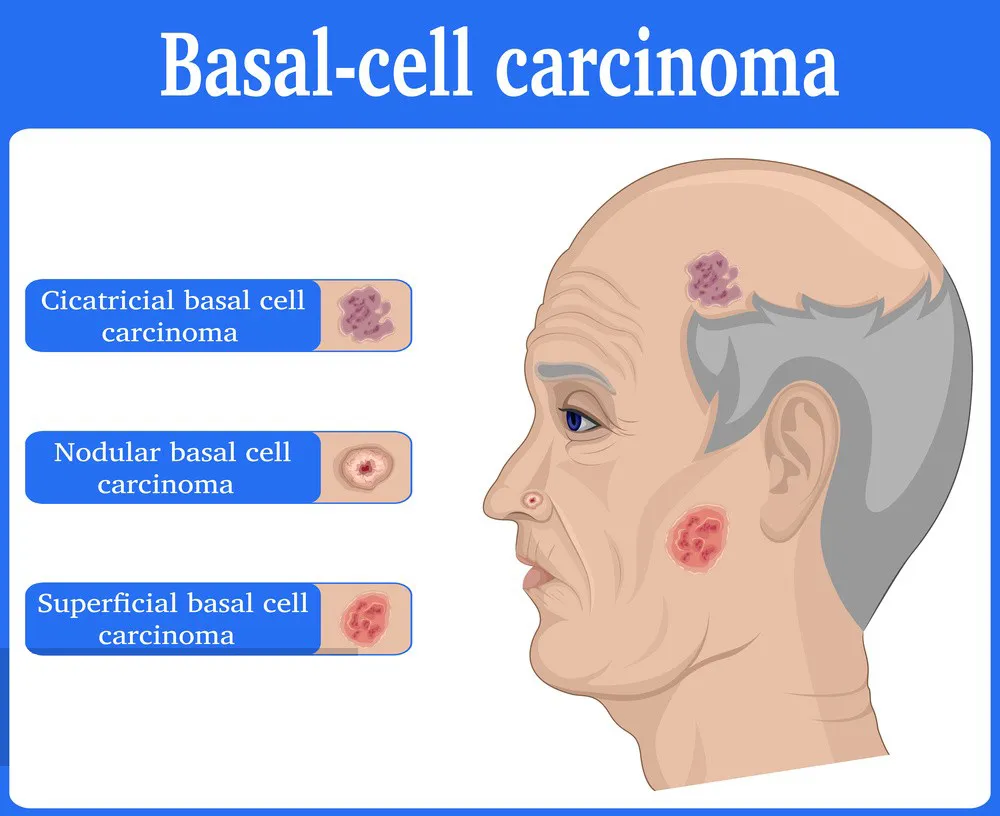
Medical Dermatoscopes are widely used in dermatology to diagnose various skin lesions, including but not limited to benign and malignant skin tumors, such as melanoma (a type of skin cancer); inflammatory skin diseases like psoriasis or eczema; and infectious skin diseases like fungal infections. The use of Medical dermatoscopes improves diagnostic accuracy and aids in the early detection and treatment of skin conditions, making them an indispensable tool for dermatologists.
How Does A Medical Dermatoscope Work?
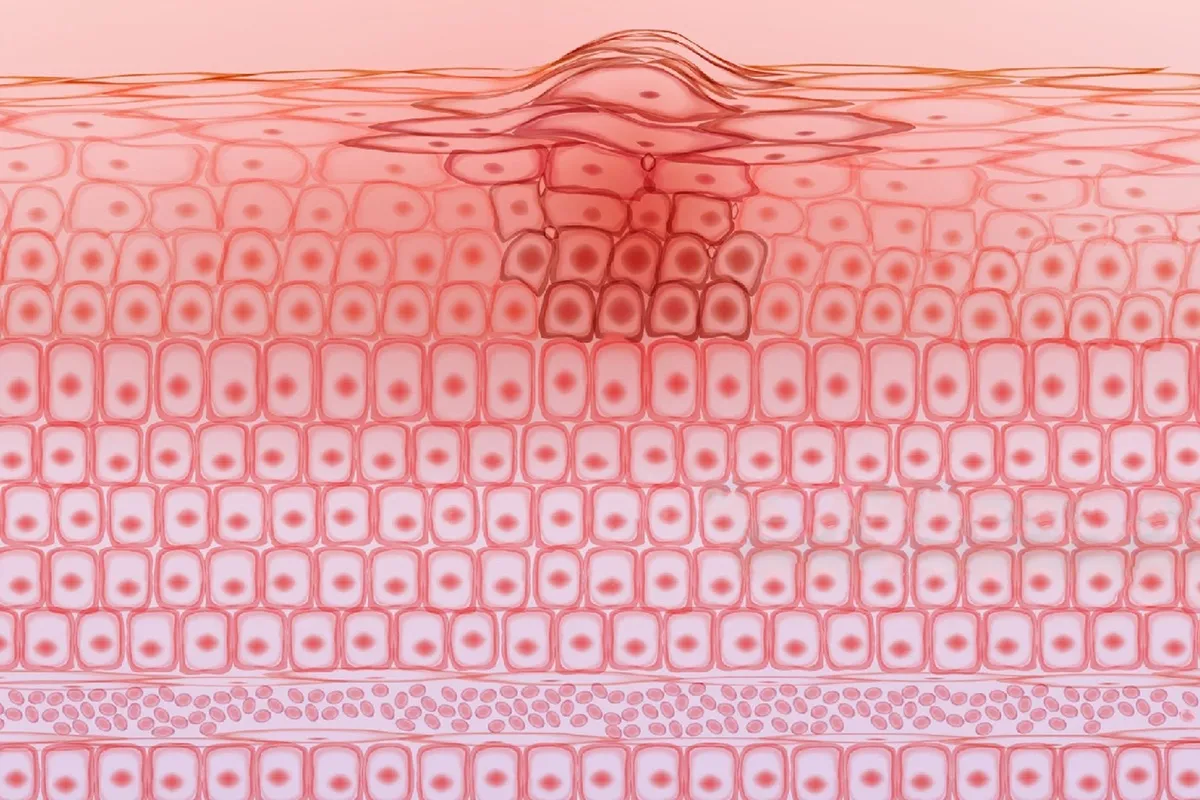
Dermoscopes enhance a doctor's ability to view tiny skin lesions through a built-in magnifying glass and light source. The light source not only illuminates the skin surface but also reduces surface reflection through polarized light technology, allowing doctors to more clearly observe deeper structures such as blood vessels and pigmentation. Cross-polarized light technology makes deeper structures more visible by using two vertically oriented polarizing filters to suppress scattered light. Modern dermatoscopes may also have digital imaging capabilities, allowing doctors to capture and store high-resolution images for further analysis and documentation. In addition, some advanced dermoscopes use spectral imaging technology to analyze the reflection and absorption of different wavelengths of light on the skin to provide detailed information about lesions. These features make dermoscopy an important tool for non-invasive skin examination, assisting doctors in making preliminary diagnoses, especially in distinguishing between benign and malignant skin lesions. Medical dermatoscopes play a vital role in medical education and training, helping medical students and physicians learn how to identify and diagnose various skin conditions.
Types of Medical Dermatoscopes
- Handheld Medical dermatoscopes
- Handheld Medical dermatoscopes with a light source
- Polarized light Medical dermatoscopes
- Cross-polarized light Medical dermatoscopes
- Digital Medical dermatoscopes
- Spectroscopic Medical dermatoscopes
- Portable Medical dermatoscopes
- High-resolution Medical dermatoscopes
- Medical Dermatoscope accessories
- Medical Dermatoscope software
- Medical Dermatoscopes with skin analysis systems
The Most Suitable Dermatoscopes for Dermatologists
The most suitable type of dermatoscope for dermatologists typically depends on various factors, including personal preferences, budget, equipment configuration in the clinic, and the types of skin lesions they need to diagnose. Some features that dermatologists may prioritize in a dermatoscope include:
- High-magnification dermoscopy allows observation of tiny skin lesions.
- Medical dermoscopy high-resolution imaging provides clear images for easy analysis and documentation.
- Polarized and cross-polarized light reduce surface reflections and enhance the visibility of deeper structures.
- Digitalization and computer integration, seamless integration with computer systems, enabling image storage, management, and remote consultation.
- Portability makes it easy to transport and use in different locations.
- Durable and reliable, the design is rugged and easy to maintain.
- Easy to use, with an intuitive interface for quick adoption by physicians.
Medical Dermoscope User Guide
Turn on the dermatoscope light source and adjust the brightness as needed to ensure even irradiation of the skin. Adjust the magnification of the dermoscope to the desired depth of the skin structure you want to observe. If the dermatoscope has polarized light, adjust the polarization as needed to reduce surface reflections. Gently bring the dermatoscope lens into contact with the skin or keep a certain distance to avoid pressure deformation. Carefully observe the surface and deep structure of the skin, noting any abnormal pigment distribution, blood vessel patterns, skin texture, etc. If the dermoscope has digital imaging capabilities, images are captured and saved for recording and further analysis. Compare your observations to normal skin structure or previous images to identify any changes.
Proper use of medical dermatoscopes can not only improve diagnostic accuracy but also provide patients with better medical services. With the above, dermatologists can effectively utilize dermoscopy to diagnose and monitor skin lesions.
People May Ask
Dermoscopy is a non-invasive, in-vivo technique that has been traditionally helpful for the examination of suspected skin lesions. It is sometimes referred to as dermatoscopy, epiluminescence microscopy, or skin surface microscopy.
Dermoscopy can help diagnose melanoma more accurately, but it cannot take the place of a histopathologic examination. Even with dermoscopy, many lesions-particularly early melanomas-may be difficult to diagnose because they lack distinct dermoscopic characteristics.
Generally speaking, moles are benign. They might develop wrinkles, be elevated, or have hairs on them. Consult your physician if a mole changes in size or color, or if you have any discomfort, bleeding, swelling, or itching.
Dermoscopy can be used to evaluate nonpigmented skin disorders such as inflammatory diseases, in addition to improving the visualization of pigmented structures. It can also be used to identify subtle structures like vascular structures and hemorrhagic areas [2,9].
The process of dermoscopy is easy, quick, and painless. Before a dermoscopy, there is nothing you need to do. Please contact your doctor if you have any questions regarding the necessity of this test or your results.
A melanoma diagnosis is strongly suggested by a total dermoscopic score of > 5.45; this is calculated as follows: 1.3 (A score) + 0.1 (B score) + 0.5 (C score) + 0.5 (D score).
Dermoscopy can help diagnose melanoma more accurately, but it cannot take the place of a histopathologic examination. Even with dermoscopy, many lesions-particularly early melanomas-may be difficult to diagnose because they lack distinct dermoscopic characteristics.
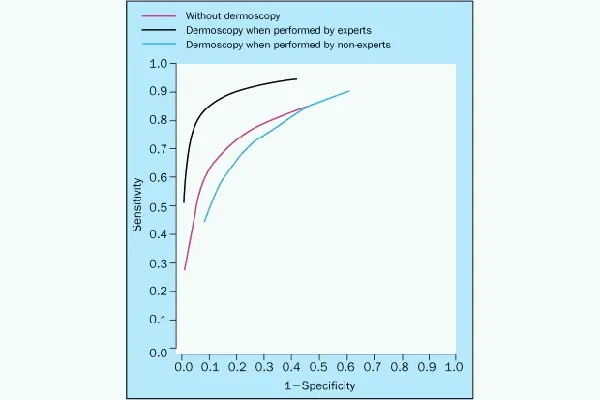
According to research, GPs may be able to more precisely identify and prioritize skin lesions, including possible skin malignancies, when they utilize dermoscopy. In the UK, however, only a small percentage of GPs use dermoscopy.
The ABCDE ruleInstead,Unbalance. One part of the skin lesion does not resemble the other in shape.Instead,border. There are jagged, notch, uneven, or fuzzy edges.Instead,Shade. There might be variations in tones of tan, brown, and black.In diameter. Typically, the diameter has increased in size or is greater than six millimeters (mm).Changing.
Dermoscopy dates back to the middle of the modern era, with significant contributions by Ernst Karl Abbe, Unna, Muller, Saphier, and others, as well as Borel's discovery (1655–1656) that lay the groundwork.
Medical Dermatoscope Products

With its 8 LED magnifying endoscope camera and carrying case, this USB digital microscope can magnify objects 40X to 1000X. It is compatible with Android, Windows 7, 8, 10, 11, Linux, and Mac.

ODM examination tools, odontomed2011 ® dermatalogy dermatoscope ^肤
Dermatoscope DELTA 20 W / handle and charger EA k-256.20.420tl (1043782) Heine Made in the USA LTD., sold separately

a brand-new, expert dermatological skin examination Skin instrument: dermoscope set

3Gen Lumio Wooden Examination Lamp for Skin Dermatology and UV Polarization

Zyrev Otoscope Oph Diagnostic Set: 34-piece Educational and Professional Setting Otoscope/Opthalmoscope Kit for Students in Medicine and Nursing with Plastic Case (Advanced)

The Best Quality Dermal Instruments for Professional Dermatology Skin Diagnosis with G.S. New Professional Set

Zyrev ZetaLife Otoscope: Lighted Otoscope, Pocket-Sized Ear Infection Detector, Available in More Than Ten Colors! (Inky)

Woods Lamp Ringworm Detection Light, Magnifying Wood Lamp, Wood S Lamp for Skin Testing, I0DO Woods Lamp Skin Analyzer Professional

Diagnostic Instruments for Skin Examination in Black Color: DDP Dermatology Dermatoscope Set
Hot Products
News & Blog
Top Reviews
many applications. Professional grade laryngoscope, opthalmoscope, and otoscope
It took some getting used to. In an instant, the ear picking tool transitioned from a blind pick to an image screen. I can see exactly what's happening in my ear through the screen, even if I'm not comfortable using the gadget just yet. Unlike an endoscope, which can only detect the depth of an ear's discomfort, this device can detect my ear congestion in advance. Even if the earspoon has a light, I'm used to caring for my ears during the day. ????Note: There is an integrated screen that can be used by pushing buttons. ????If the display was touch-enabled and full-screen, this visual ear cleaner would have greater power.
I haven't use it yet, but looks good, seems good materials and quality, I'll come back to this review when I try it.