Case for iPhone – IBOOLO
People May Ask
The preferred medication for managing scabies is permethrin. When dealing with crusted scabies, it is recommended to apply topical permethrin every 2-3 days for a duration of 1-2 weeks. As a substitute topical agent, 25% Benzyl benzoate, either with or without the addition of tea tree oil, can be utilized as an alternative to permethrin.
The progression of melanoma is rapid, posing a significant risk to life within a short span of six weeks. Furthermore, without proper treatment, it has the potential to disseminate to various regions of the body.
Although most moles do not necessitate medical intervention, there may be instances where you might desire to have one removed due to dissatisfaction with its appearance or sensation. If you harbor any concerns regarding a mole, it is advisable to consult with your healthcare professional. Typically, moles are excised when there is suspicion of malignancy or for aesthetic purposes.
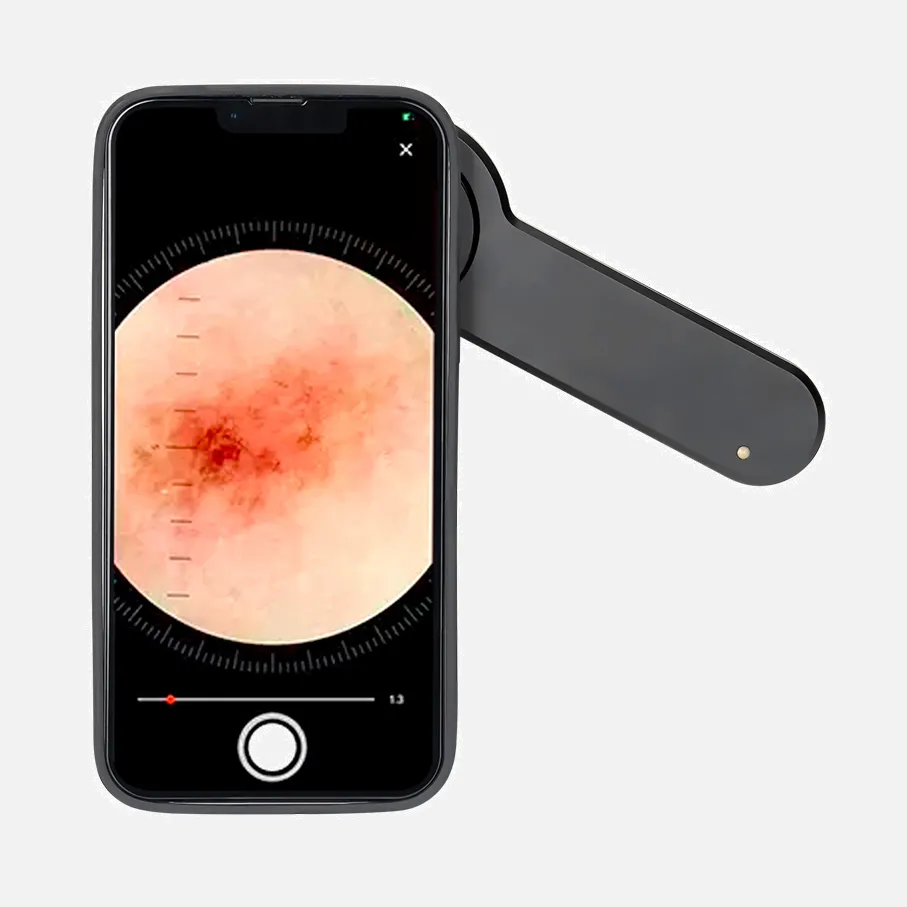
Capturing clinical imagery
For an introductory shot: position yourself approximately 1 meter from the targeted area and capture the photograph. ...
For a magnified image: adjust your camera's position to about 10-12 centimeters away from the skin condition. ...
Capturing a side view of an elevated lesion is crucial: in cases where the lesion is elevated, a side-angled photograph can be immensely beneficial (refer to figure 4)
Date:
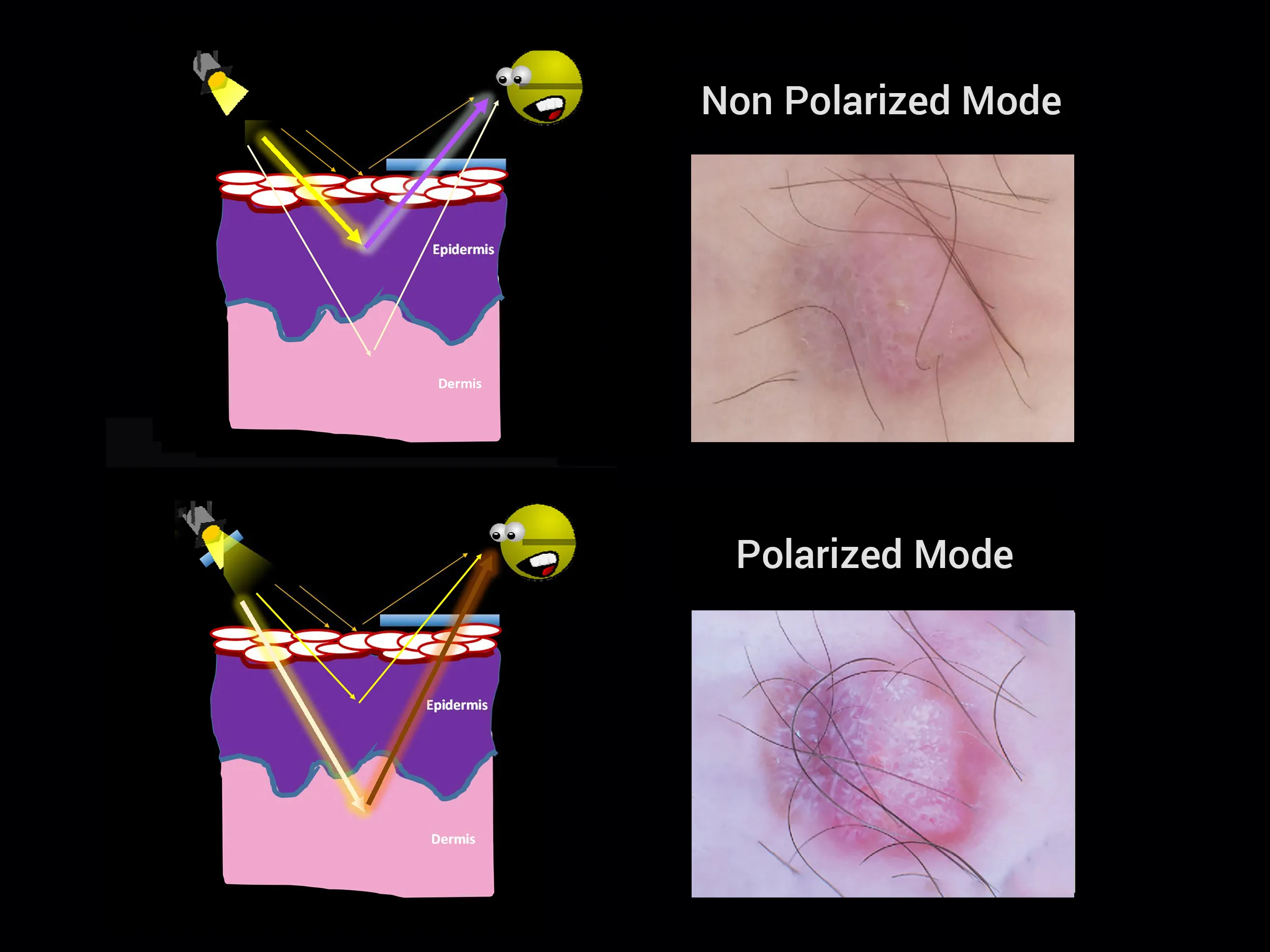
When compared solely to visual inspection, incorporating dermoscopy into the examination process enhanced sensitivity, raising it from 67% to 85% (across 5 studies involving 4455 lesions; P = .0001). Additionally, it also bolstered specificity, lifting it from 97.2% to 98.2% (within 3 studies encompassing 3721 lesions; P = .006). However, it's worth noting that these findings were constrained by notable variations across the different studies.
The vast majority (close to 100%) of individuals diagnosed with stage 1 melanoma skin cancer are expected to live with their cancer for a duration of five years or beyond. Similarly, approximately 85 out of every 100 individuals (around 85%) with stage 2 melanoma skin cancer are anticipated to survive their cancer for five years or longer following their diagnosis.
Summary. Context: Dermoscopy, a non-intrusive technique, has gained popularity for enhancing the precision of general dermatological condition diagnoses. Aim: To identify dermoscopic characteristics and their diagnostic significance in differentiating between prevalent inflammatory and infectious skin diseases. January 24th, 2023
Indications of metastatic melanoma apart from a mole
Lungs – Persistent coughing or feeling breathless. Brain – Experiencing headaches or seizures. Lymphatic System – Noticeable enlargement of lymph nodes. Liver – Decreased appetite or inexplicable weight reduction.
In general, moles are considered non-threatening and pose no significant concern. Unless a mole exhibits cancerous characteristics, there is no need for removal unless it becomes bothersome.
Without insurance coverage, a skin biopsy often ranges from $120 to $450 in cost. Additional lab evaluation expenses may incur, varying from $50 to $350. Is a biopsy necessary, despite our perceived diagnosis? This ultimately hinges on the specifics of your skin condition.