Case for iPhone – IBOOLO
People May Ask
Within the study group, 43 individuals attained full remission (CR) during the observational period, contrasted with 83 who failed to do so. Amongst the 83 patients who did not reach CR, 35 showed some degree of improvement, while 48 either exhibited no improvement or saw their condition deteriorate. The median duration to attain CR was recorded as 46 months, with a standard deviation of 18.8 months.
Initially, you may commence by consulting with your general practitioner or dental practitioner. It's noteworthy that individuals afflicted with oral lichen planus can also exhibit manifestations of the condition on their skin. Consequently, based on the specific symptoms you exhibit, you might be directed to seek the expertise of a specialist in skin disorders, known as a dermatologist, or a gum and dental health specialist, commonly referred to as a periodontist.
The ailment frequently exhibits a tendency to gradually resolve on its own, albeit this process commonly spans from several months to years. Therapeutic interventions exist that are designed to alleviate the bothersome symptoms of itching, while simultaneously aiming to halt the progression of damage to hair follicles. What constitutes effective treatment strategies for lichen planopilaris?
Certain possible consequences of lichen planopilaris encompass: Irreversible hair loss, also known as cicatricial alopecia: This condition may lead to the irreparable damage of hair follicles, ultimately causing scarring and the permanent absence of hair in the affected sections of the scalp. As of May 1, 2024.
A study on 34006 individuals revealed a significant prevalence of Vitamin D insufficiency among patients diagnosed with lichen planopilaris and frontal fibrosing alopecia. The essentiality of Vitamin D in facilitating calcium assimilation, maintaining skin equilibrium, and modulating immune responses is well-established. Furthermore, it emerges as a vital factor in supporting the healthy development and cyclical activity of hair follicles.
I am routinely inquired about whether individuals suffering from lichen planopilaris (LPP) and comparable scarring hair loss conditions can safely color their hair. The consensus among experts is that for a vast majority of patients with scarring alopecia, the application of permanent, semi-permanent, or even temporary hair dyes poses no significant risk.
Clobex shampoo, formulated with clobetasol proportionate, serves as an illustrative example of a steroid-based shampoo. This particular shampoo effectively alleviates inflammation associated with LPP, with some of my patients opting for a twice-weekly application during LPP flare-ups, while others adopt a once-every-two-weeks regimen when the condition is more stabilized.
What are the treatment options for lichen planopilaris?
Antibiotics are prescribed to combat bacterial infections and alleviate inflammatory symptoms.
Anti-malarial medications, traditionally used for malaria, can also aid in managing certain inflammatory skin disorders.
Corticosteroids play a crucial role in regulating inflammatory responses.
Low-intensity laser therapy employs targeted light waves for the management of skin inflammation.
Additional modalities are also available...•
Summary. Context: Lichen planopilaris (LPP), a form of lichen planus that specifically affects hair follicles, presents a challenge in diagnosis due to a recently identified subtype that can mimic androgenetic alopecia (AGA), thus potentially leading to misdiagnosis.
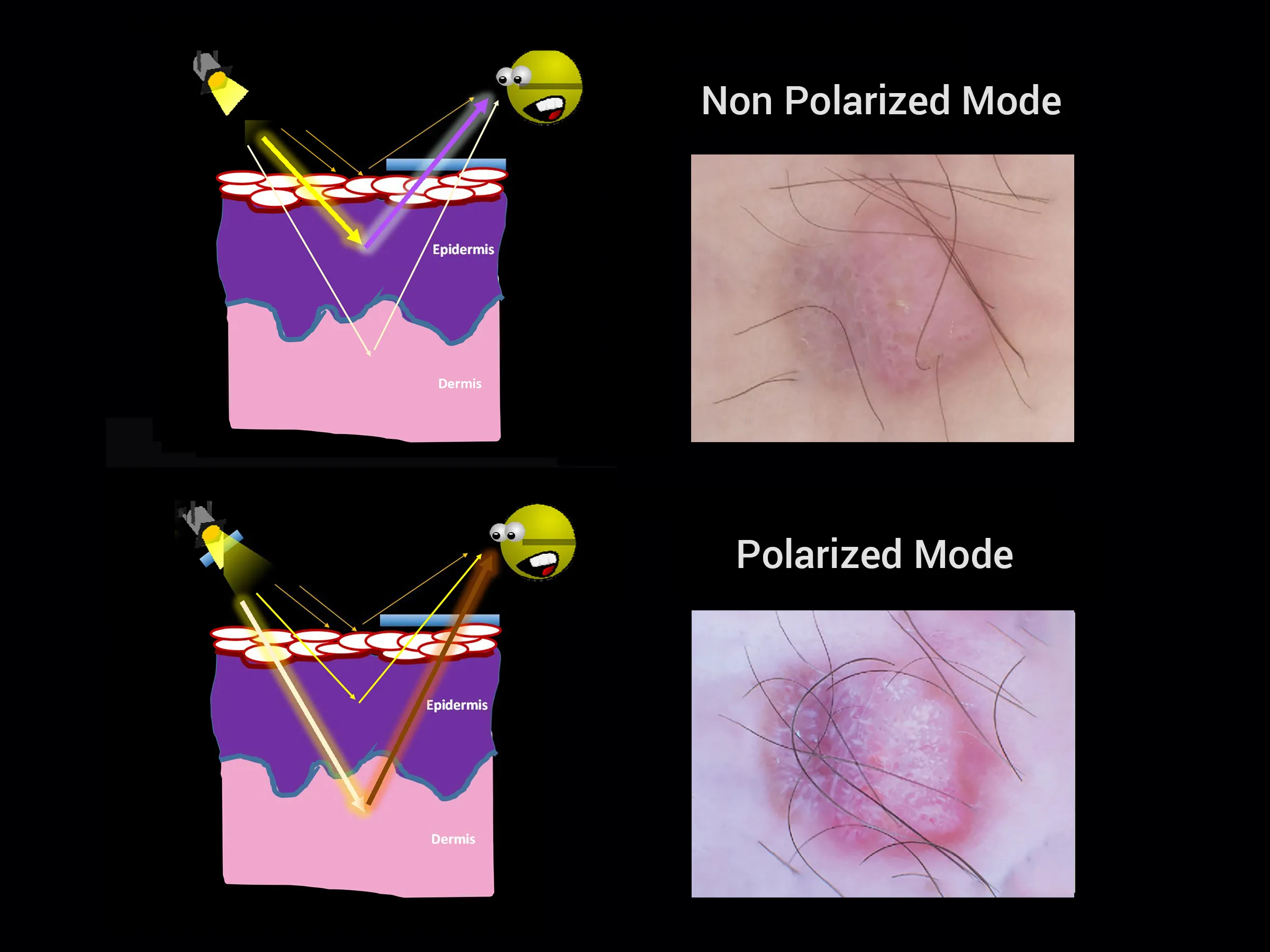
The primary differential diagnoses for LPP encompass conditions such as discoid lupus erythematosus, alopecia areata, centrifugal cicatricial alopecia, and folliculitis decalvans. A thorough physical evaluation, coupled with dermoscopic and histological analyses, plays a pivotal role in distinguishing LPP from these aforementioned conditions. February 27th, 2018