Article
Acral Melanoma Dermoscopy
Acral melanoma is a special subtype of skin cancer. Late presentation of patients and delayed diagnosis by doctors result in poor prognosis and survival. Despite advances in the understanding of the key features of this disease, early diagnosis of acral melanoma remains challenging. A combination of clinical presentation, dermoscopy, and histologic findings is essential for…
Acral Melanoma Dermoscopy: Precision Skin Monitoring | IBOOLO
Unlock early detection with IBOOLO’s advanced acral melanoma dermoscopy tools. High-quality dermatoscopes from trusted suppliers offer clear imaging for palms, soles, and nails. Monitor skin health confidently with professional-grade devices, paired with expert medical guidance.
Understanding Acral Melanoma Dermoscopy with IBOOLO
Acral melanoma dermoscopy is a vital tool for observing skin changes in hard-to-detect areas like the palms, soles, and under nails. Offered by trusted suppliers like IBOOLO, advanced dermatoscopes enhance the ability to monitor this rare subtype of melanoma. These devices serve as auxiliary observation tools, providing high-resolution imaging to track skin irregularities, always in conjunction with professional medical advice to ensure accurate interpretation.
What Is Acral Melanoma and Why Is Dermoscopy Essential?
Acral melanoma, also known as acral lentiginous melanoma, is a rare form of skin cancer that appears on the palms, soles, or under the nails—areas not typically exposed to sunlight. Unlike other melanomas often linked to UV exposure, acral melanoma affects individuals across all skin types, with a higher prevalence in darker-skinned populations. Its hidden locations make early detection challenging, often leading to discovery at advanced stages. Acral melanoma dermoscopy, using devices from trusted suppliers like IBOOLO, provides magnified, illuminated views of skin structures, revealing details invisible to the naked eye. This non-invasive technique helps users observe patterns and changes, supporting timely consultations with dermatologists. While dermatoscopes are not diagnostic tools, their precision aids in identifying concerning features, fostering proactive skin health monitoring when paired with professional expertise.
Why Is Diagnosing Acral Melanoma Challenging?
Diagnosing acral melanoma presents unique challenges due to its atypical presentation and misconceptions about its occurrence. These factors often delay detection, making tools like acral melanoma dermoscopy critical for improving outcomes. Below are the primary difficulties:
- Atypical Appearance: Early acral melanoma lesions often mimic benign moles, with pigmentation following the ridges of the palms or soles, leading to irregular borders and asymmetry that can be mistaken for non-cancerous conditions.
- Misconceptions About Location: Many believe melanoma only occurs in sun-exposed areas, causing neglect of changes in non-sun-exposed regions like the soles or under nails, delaying identification.
- Histopathological Complexity: Biopsies of acral melanoma may not always show typical cancer cell characteristics, increasing the risk of misinterpretation during histopathological analysis.
Acral melanoma dermoscopy, as offered by IBOOLO’s advanced devices, helps overcome these challenges by providing clear visuals of subsurface skin structures. This allows users to monitor irregularities like pigment distribution or vascular patterns, which can prompt earlier professional evaluation when used as an auxiliary tool.
How Does Acral Melanoma Dermoscopy Improve Detection?
Acral melanoma dermoscopy enhances detection by offering a non-invasive, detailed view of skin lesions, making it easier to spot subtle changes that may indicate malignancy. Devices like IBOOLO’s DE-3100 and DE-4100 dermatoscopes use polarized and non-polarized light to reveal critical features such as pigment patterns and vascular structures. This technology supports observation of skin irregularities without invasive procedures, reducing the need for unnecessary biopsies while minimizing infection risks. Key benefits include:
- Enhanced Visualization: Dermoscopy magnifies skin features up to 30x, revealing details like irregular pigmentation or atypical vascular patterns that are not visible without specialized equipment.
- Image Capture Capabilities: Modern dermatoscopes, compatible with smartphones or cameras, allow users to store images for ongoing monitoring or sharing with healthcare professionals.
- Non-Invasive Monitoring: Polarized non-contact modes enable examination of sensitive or hard-to-reach areas like nails, avoiding discomfort or cross-contamination.
While acral melanoma dermoscopy is a powerful observation tool, it requires professional medical input to interpret findings accurately. By using high-quality dermatoscopes from trusted suppliers, users can track changes effectively, supporting early consultation with dermatologists for further evaluation.
What Are the Key Dermoscopic Features of Acral Melanoma?
Acral melanoma dermoscopy provides critical visual clues to distinguish malignant lesions from benign ones, such as acral nevi. IBOOLO’s dermatoscopes highlight specific patterns that aid in observation. Key dermoscopic features include:
- Parallel Ridge Pattern: Irregular pigmentation following the ridges of the palms or soles, often disrupted or uneven.
- Irregular Diffuse Pigmentation: Uneven color distribution with multiple shades, such as brown, black, or blue-gray.
- Multiple Colors: Presence of varied colors, including red, within the lesion, indicating potential malignancy.
- Irregular Dots and Globules: Scattered, non-uniform dots or globules of varying sizes and colors.
- Atypical Vascular Patterns: Unusual or irregular blood vessel structures within the lesion.
- Asymmetrical Borders: Uneven, notched, or blurred edges, contrasting with the symmetry of benign lesions.
These features, observed through acral melanoma dermoscopy, help users identify concerning changes. However, professional medical advice is essential to interpret these observations, as dermatoscopes are auxiliary tools, not diagnostic devices.
How Can You Distinguish Acral Melanoma from Acral Nevus?
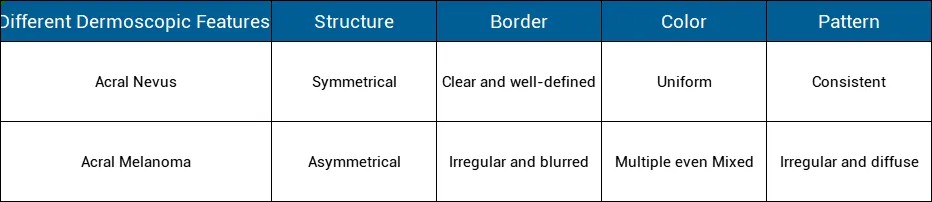
Distinguishing acral melanoma from benign acral nevi (melanocytic moles) is critical for effective monitoring. Acral melanoma dermoscopy plays a pivotal role by highlighting differences in structure and appearance. Acral nevi typically show uniform pigmentation, symmetrical shapes, and regular patterns, such as parallel furrow patterns. In contrast, acral melanoma often exhibits irregular pigmentation, asymmetry, and disrupted patterns like the parallel ridge pattern. IBOOLO’s dermatoscopes, with advanced optics and lighting, make these distinctions clearer, enabling users to monitor changes and seek professional evaluation when needed. Regular self-examinations with a dermatoscope, combined with professional consultations, enhance the ability to differentiate these conditions, ensuring timely action for any suspicious findings.
What Factors Affect Acral Melanoma Prognosis?
The prognosis of acral melanoma is often impacted by late detection, but several factors influence outcomes. Acral melanoma dermoscopy can aid in early observation, but professional assessment remains crucial. Key factors include:
- Lesion Size and Location: Lesions larger than 4mm or in weight-bearing areas like soles or under nails are harder to detect early, potentially worsening prognosis.
- Ulceration: Ulcerated lesions are associated with more advanced stages compared to non-ulcerated ones.
- Thickness: Thicker tumors (greater Breslow depth) indicate deeper invasion, often linked to poorer outcomes.
- Stage at Detection: Advanced stages, with spread to lymph nodes or other areas, significantly reduce survival rates.
- Age and Gender: Older individuals and males tend to have worse outcomes than younger individuals or females.
- Genetic Mutations: Mutations like BRAF, KIT, or NRAS can influence prognosis and response to targeted therapies.
- Immune System Health: A compromised immune system may contribute to poorer prognosis.
Using acral melanoma dermoscopy, such as IBOOLO’s portable devices, supports early observation of these factors, encouraging timely medical consultations to address potential concerns.
How Can Acral Melanoma Detection Be Improved?
Improving the detection of acral melanoma requires a combination of awareness, regular monitoring, and advanced tools like acral melanoma dermoscopy. Here are practical steps to enhance detection:
- Increase Public Awareness: Educate individuals about the risk of melanoma in non-sun-exposed areas, emphasizing the need to check palms, soles, and nails.
- Regular Self-Examinations: Use a high-quality dermatoscope, like those from IBOOLO, to routinely inspect skin for unusual spots or changes, especially in high-risk areas.
- Professional Dermoscopy Use: Consult dermatologists who use advanced dermatoscopes for detailed examinations when suspicious lesions are identified.
- Leverage Technology: Utilize dermatoscopes with image capture and software integration to track changes over time and share visuals with healthcare providers.
By incorporating acral melanoma dermoscopy into regular skin checks, individuals and professionals can enhance early detection efforts. Devices from trusted suppliers like IBOOLO, with features like polarized light and smartphone compatibility, empower users to monitor skin health effectively, always in collaboration with medical experts to ensure accurate interpretation and follow-up.
Recommended reading
Can dermoscopy with an electronic dermatoscope detect cancer?
Clinical studies validate that quality electronic dermatoscopes allow users to visually detect many early signs of skin cancer development with accuracy approaching in-person expert analysis. Features like asymmetry, border irregularity, evolving diameter, new colors, etc. can be recognized using an electronic dermatoscope. So combining vigilant self-checks with an electronic dermatoscope s photo documentation capabilities greatly aids early stage non-melanoma and melanoma detection.
portable Dermoscopy power
Traditional dermatoscopes tend to be bulky desktop devices restricted to clinical settings. In contrast, today s handheld dermatoscopes enable portable dermoscopy anywhere. powered by batteries, these mobile phone dermatoscopes and compact handheld dermatoscopes free users from requiring an electrical outlet. Their lightweight, pocket-sized design allows easy whole-body examination in good lighting with a handheld dermatoscope.
Who Can perform Dermoscopy?
The powerful magnification and lighting capabilities dermatoscopes offer provide beneficial visual data for everyone to understand the current state of their skin and track changes over time. However, specialized medical training is typically required to analyze dermoscopy images and determine if biopsies or treatment are necessary. Dermatologists have this expertise.
Acral melanoma is a special subtype of skin cancer. Late presentation of patients and delayed diagnosis by doctors result in poor prognosis and survival. Despite advances in the understanding of the key features of this disease, early diagnosis of acral melanoma remains challenging. A combination of clinical presentation, dermoscopy, and histologic findings is essential for the diagnosis of acral melanoma.
What is acral melanoma?
Acral melanoma is also known as acral lentiginous melanoma. Acral melanoma is a rare subtype of melanoma. And it usually happens in acral of the body, like palms on the hands, soles of the feet, and under the nails. Unlike other melanomas that is usually caused by over sun exposure and occurs in fair-skinned people . Oppositely, the places include palms, soles and under the nails are not commonly exposed on sunburn. Dark people usually don’t get melanomas. However, acral melanoma is the most common type of melanoma in dark people and it also affect people of all ethnic backgrounds. Hence these these melanomas are found later than other types of melanomas after they invade deeper layers of the skin or metastasize. So it brings more difficult to detect and diagnose the acral melanoma than other skin cancers.

What are the difficulties in diagnosing acral melanoma?
As the acral melanoma is usually found late by patients, there are some difficulties and misunderstandings in the diagnosing acral melanoma as below:
Atypical Presentation: Early acral melanoma lesions are often difficult to diagnose because the pigmentation of the lesions usually follow the skin marking on the palms and soles, resulting in asymmetrical appearance and irregular borders. This similarity with benign melanocytic moles can make early diagnosis difficult.
Misconceptions: There is a misconception that melanoma only happen on the areas exposure in sun. So people always will neglect the changes on other parts of the skin, which causes the delayed diagnosis of acral melanoma.Unfortunately, this will lead to acral melanoma being found at advanced stage and bring a poor treatment effectiveness.
Histopathological complexity: The biopsy and histopathological examination needed to diagnose acral melanoma may be very complexity. Because acral melanoma cells may not present its typical characteristics always. This lead to a potential misdiagnosis.
Advantages of dermoscopy in the diagnosis of acral melanoma
To improve the diagnosis of acral melanoma, it is crucial to use the advanced diagnosis technique dermoscopy. Dermoscopy is a handheld device equipped with a magnifying lens and a light source to allows a enhanced visual for dermatologist to diagnose skin lesions and skin conditions, like acral melanoma and other types of skin cancer. In professional hands, dermatoscope can help to diagnose the very early stage of melanoma by typical structures and patterns which can not visual by naked eyes. In addition, the dermatology is invasive and painless. It not only can avoid the cross infection during examination but also can reduce the unnecessary biopsy and surgery.
Some modern advanced dermoscopes can capture image of lesion or connect to computer software for better analysis.
What are dermoscopic features of acral melanoma?
Dermoscopy is an essential tool to help dermatologists diagnose the acral melanoma by providing critical visual clues that differentiate it from benign lesions. There are some key dermoscopic features associated with acral melanoma as below:
Parallel Ridge Pattern: This pattern is characterized by irregular and disrupted pattern that follows the ridges of the skin on the palms and soles.
Irregular Diffuse Pigmentation: Uneven distribution of pigmentation color, often with multiple shades of colors.
Multiple or Mixed Colors: Acral melanoma lesions often present a mix of brown, blue-grey, black, and red colors or multiple colors.
Irregular Dots and Globules: Exhibit of scattered dots and globules of varying size and colors within the lesion.
Atypical Vascular Patterns: Presence of unusual or irregular blood vessels within the lesion.
Asymmetrical and Irregular Border: Acral melanoma with asymmetrical structures and irregular, uneven,notched or blurred borders.
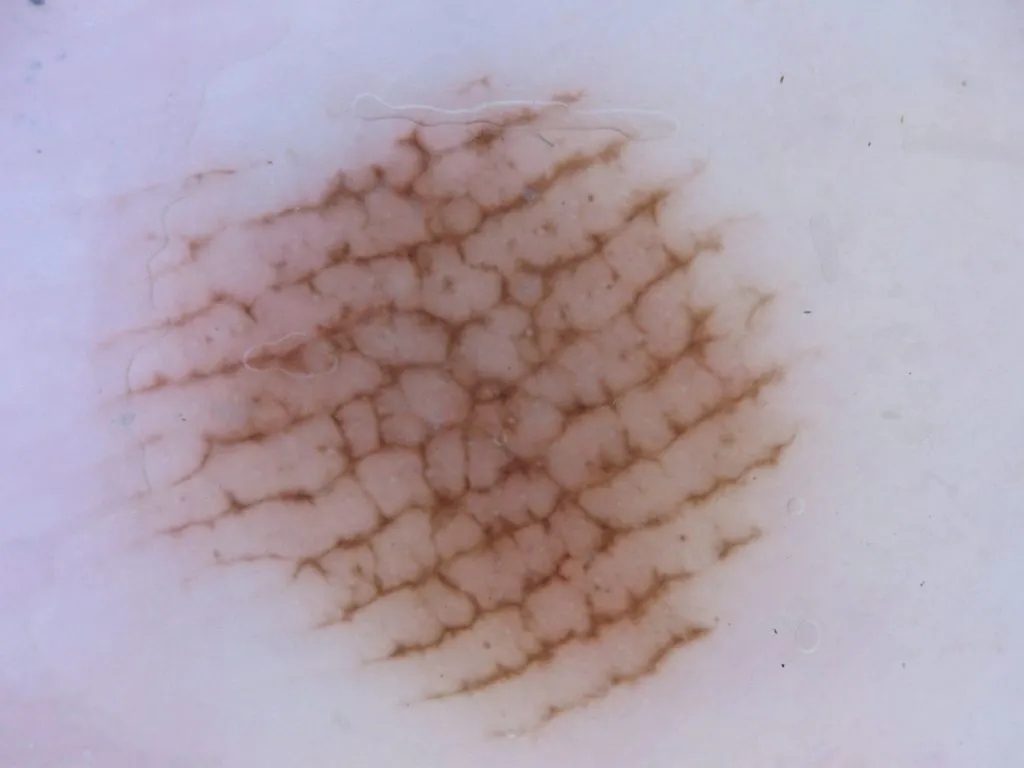
Distinguish the dermoscopic features of similar lesions like acral nevus
Acral nevus (benign melanocytic nevus) and acral melanoma may present similar characteristics. While dermoscopy is a very important and necessary tool tell the differences from them. Here are the key points for distinguishing acral nevus from acral melanoma including:
Exploring the factors affecting the prognosis of acral melanoma
Due to the late inspection and detection of acral melanoma, resulting in a poor prognosis. Except for that, there are some other factors that affect the prognosis of acral melanoma as below:
Feature of the lesion :
Size and Location: If the size of the lesion Larger than 4 mm, and those also located in weight-bearing areas like the soles or under the nails can be more challenging to detect and treat early. This means a potentially worsening prognosis.
Ulceration: Commonly ulcerated lesions are associated with a worse prognosis than the one is not ulcerated.
Thickness: Thickness is the obvious factors which affect the prognosis of acral melanoma. The thicker tumors (greater breslow depth) are often associated with a more worse prognosis.
Stage of the Lesion:
Advanced Stages: Patients diagnosed at advanced stages that means the lesion have invaded into lymph nodes or other parts of the body have a poor prognosis. Advanced stage brings more difficulties in survival rate.
Age and Gender: As reported and analysis, that the older age and the male patients generally tend to have poor prognosis than the young and the female.
Gene mutation :
Commonly gene mutation such as BRAF, KIT, NRAS,and so on, this altered genes can influence prognosis and response to targeted therapies. It causes a poor prognosis of acral melanoma.
Immune System: Especially the patients diagnosed at acral melanoma or other cancers and with low immune system tend to have a worse prognosis than the normal ones.

How to improve the diagnosis of acral melanoma?
As we know that it is difficult to detect and diagnose the acral melanoma especially in its early stage due to its special characteristics. Then how to improve the diagnosis of acral melanoma? There are some methods to improve the diagnosis of acral melanoma including:
People should raise the awareness about the possibility of melanoma in non-sun exposed areas and learn more knowledge about this rare and special skin cancer.
People should do more regular self-examinations by dermoscope, especially of the palms, soles of the feet, and under of nail if there is unusual spots or dots.
People and dermatologists should use dermoscopy, an advanced diagnostic device and techniques to inspect skin situations. Particularly, it is a must to have skin checked by dermoscopy by professional doctors when suspicious lesions are found.
As we can see, early detection are very important to improve the prognosis of acral melanoma. Dermoscope indeed plays a vita role in detecting, diagnosing, monitoring and managing skin lesions and skin cancers like acral melanoma. Dermoscopy is a very valuable and helpful device in the field of dermatology, significantly increasing the ability to inspect and diagnose acral melanoma in early stage. Dermoscopy not only improves patient confidence through early intervention and appropriate treatment schedule, dermoscopy but also reduce the infection during the examination.






















