Article
Dermoscopy of Actinic Keratosis
Actinic keratosis is a very common skin diseases. It is a major growing public health problem especially among older adults in white. A meta-analysis of observational studies reported by British Association of Dermatologists showed that the overall prevalence of actinic keratosis worldwide was 14%, with an estimated incidence of 1,928 cases per 100,000 people per…
Actinic Keratosis Dermoscopy: A Clinical Guide to Solar and Pigmented Keratosis
In modern dermatology, the dermoscopy of actinic keratosis has emerged as an indispensable non-invasive tool for early intervention. Actinic keratosis, commonly known as solar keratosis, is a precancerous intraepidermal proliferation of atypical keratinocytes caused by cumulative ultraviolet exposure. Without precise diagnosis, these lesions carry a significant risk of progressing into invasive squamous cell carcinoma (SCC).
At IBOOLO, we recognize that effective management begins with high-resolution imaging. This guide explores the hallmark patterns, technological requirements, and clinical nuances of actinic keratosis dermoscopy to empower clinicians in providing accurate, life-saving care.
Dermoscopy of Actinic Keratosis: The Strawberry Pattern
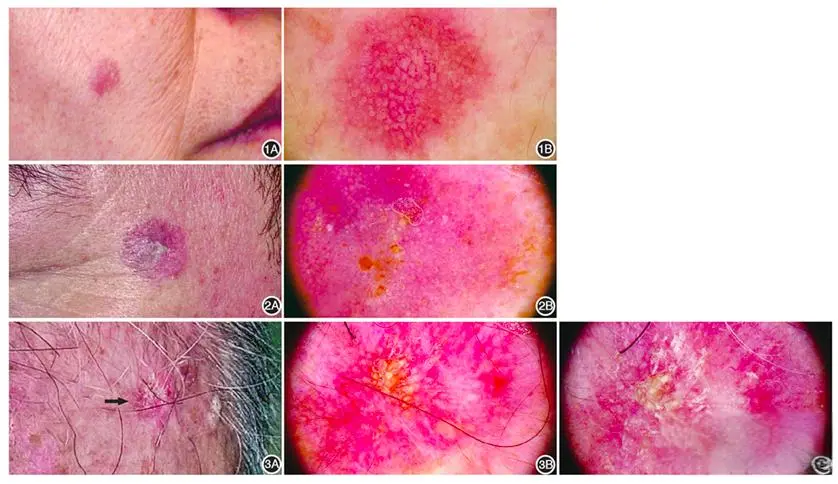
The most recognizable hallmark in the dermoscopy of actinic keratosis is the "strawberry pattern." This clinical marker consists of a diffuse erythematous pseudonetwork created by reddish-pink wavy vessels surrounding yellowish-white, keratotic follicular openings.
During a comprehensive dermoscopy actinic keratosis screening, clinicians typically identify the following key features:
- Keratotic Scales: Surface white or yellowish scales reflecting disordered keratinization.
- Prominent Follicular Openings: Often filled with keratotic plugs and surrounded by a white-yellowish halo.
- Red Pseudonetwork: A characteristic background hue that distinguishes AK from normal skin pigmentation.
Pigmented Actinic Keratosis Dermoscopy: Managing Melanoma Mimickers
One of the most complex clinical scenarios is pigmented actinic keratosis dermoscopy. This variant often presents a diagnostic challenge as it can closely mimic lentigo maligna or melanoma. In these cases, the pigment is typically distributed as fine gray-brown dots or granules around the follicular openings.
Successful pigmented actinic keratosis dermoscopy requires identifying subtle clues such as:
- Annular-Granular Patterns: Minute dots forming rings around the hair follicles.
- Rhomboidal Structures: Pigment deposits that coalesce around follicular openings as the lesion evolves.
- Rosettes: Four-dot crystalline structures visible under polarized light, indicating advanced solar damage.
Differentiating Solar Keratosis from Squamous Cell Carcinoma
A primary objective of solar keratosis dermoscopy is to monitor for signs of malignant transformation into SCC. While AK presents with thin white scales and a red pseudonetwork, progression is often marked by the appearance of glomerular vessels and thick keratin masses.
| Dermoscopic Feature | Actinic Keratosis (AK) | Squamous Cell Carcinoma (SCC) |
|---|---|---|
| Vascularity | Red Pseudonetwork | Atypical / Polymorphous Vessels |
| Scale Type | Fine, Yellow-White Scales | Thick Keratin Plug / Central Crust |
| Follicular View | Strawberry Pattern | Opaque / Disrupted Follicles |
Enhancing Solar Keratosis Dermoscopy with IBOOLO Optics
The accuracy of solar keratosis dermoscopy is fundamentally tied to the quality of the lens and the lighting system. IBOOLO professional dermatoscopes, such as the DE-4100 series, utilize cross-polarization to eliminate surface glare, allowing clinicians to see deeper into the dermal structures without the need for interface fluids.
By integrating high-resolution imaging with smartphone compatibility, our devices enable "Sequential Digital Dermoscopy Imaging." This allows for the long-term monitoring of actinic keratosis dermoscopy findings, tracking treatment efficacy post-cryotherapy or topical intervention. Precision optics ensure that subtle annular-granular structures in pigmented actinic keratosis dermoscopy are visualized with absolute fidelity.
Mastery of actinic keratosis dermoscopy is essential for effective skin cancer prevention. From identifying the early strawberry pattern to managing complex pigmented lesions, the right technology empowers clinicians to provide the highest standard of care.
Recommended reading
China 365nm UV Lamp Manufacturer & Factory Provides Affordable Products for Clients - IBOOLO
As a leading 365nm UV Lamp manufacturer & factory in China, we specialize in affordable products to meet our clients' unique needs. Our skilled engineers can modify designs or create new UV lamps from scratch.
Verification of Conformity – IBOOLO
Shenzhen Iboolo Optics Co.Ltd has been specialized in researching and manufacturing industrial Woods Lamp, Dermatoscope, Macro lens and Microscope, since 2012. As a professional dermatoscope supplier, we have excellent teams who focus on products development & design, quality control & inspection and company running.
Wholesale Back-up Battery for DE-3100 suppliers & factories – IBOOLO
IBOOLO is a Wholesale Back-up Battery for DE-3100 suppliers & factories. Information for Back-up Battery for DE-3100: Back-up Battery for DE-3100 Dermatoscope...
Actinic keratosis is a very common skin diseases. It is a major growing public health problem especially among older adults in white. A meta-analysis of observational studies reported by British Association of Dermatologists showed that the overall prevalence of actinic keratosis worldwide was 14%, with an estimated incidence of 1,928 cases per 100,000 people per year.
People in geographic locations with too much sun exposure are more likely to have actinic keratosis. Because there is a increasing tend that actinic keratosis translates into an risk of skin cancer, especially squamous cell carcinoma. Identifying patients at high risk for actinic keratosis and for timely and effective treatment of actinic keratosis are very important.
With the development of medical equipment, a small and flexible skin inspection tool, the dermoscope, emerged. Dermoscopy plays a crucial role in the early diagnosis, evaluation and treatment of actinic keratosis. Dermoscopy of actinic keratosis helps dermatologists make more timely and accurate analysis and judgment.Dermoscopy of actinic keratosis also enhances the confidence of doctors and patients in the treatment of actinic keratosis. Dermoscopy of actinic keratosis allows actinic keratosis to be treated more effectively.

What is Actinic Keratosis?
Actinic keratosis (shorted call AK) is also know as solar keratosis. Actinic keratoses are very common, and many people have them. It is a skin disease usually caused by long time exposure to ultraviolet light from the sun. The disease may require medical intervention, including medication or surgery, to reduce symptoms and prevent further deterioration. The best way to prevent solar keratosis is to avoid excessive exposure to the sun.
What are the Clinical Features of Actinic Keratosis?
Actinic keratosis disorders the skin to appear in thick, rough patches, itching or burning, raised wart-like growth, tenderness or pain, inflammation, increased size or thickness, multiple lesions. Actinic keratosis usually occurs in areas frequently exposed to sunlight, such as the head, arms, ears, scalp, neck, hands, face, etc.



Causes of Actinic Keratosis
It is a high risk of solar keratosis to exposure to ultraviolet (UV) radiation from the sun in long time. There are also other factors resulting in solar keratosis as below:
Long-term sunlight exposure: Long-term exposure to ultraviolet radiation from the sun is the main factor of solar keratosis.
Fair skin: People with fair skin are more susceptible to actinic keratosis. Because fair skin is more easily to receive more harmful effects of UV radiation.
Age: Actinic keratos is more commonly occurs in the middle age and old age people. Because accumulated sun exposure over time increases the posibility of developing these lesions.
History of sunburn: Severe sunburn, particularly in childhood or adolescence, increases the risk of developing actinic keratosis later in life.
Weakened immune system: Conditions or medications that weaken the immune system may also contribute to the development of solar keratosis, as the body may not be able to repair skin damage caused by UV light.
High risk Groups and Evolution
People in white, the elderly, and outdoor workers etc, are high-risk groups for actinic keratosis.
Actinic keratosis is considered a precancerous lesion because if left untreated, it can develop into skin cancer, especially squamous cell carcinoma. It is important to evaluate actinic keratosis lesions by a dermatologist and treat solar keratosis promptly to reduce the risk of skin cancer.
Dermoscopy of Actinic Keratosis
The application of dermoscopy of actinic keratosis
Dermoscopy is a non-invasive tool used to examine skin lesions. There are some main applications of dermoscopy of actinic keratosis like below:
Improved visualization: Dermatoscopy allows dermatologists to examine solar keratosis lesions more clearly, like the morphological and structural details of the lesions.
Early detection: Dermoscopy helps early detection of solar keratosis lesions for timely intervention and treatment. Early detection is essential to prevent the progressing of actinic keratoss to skin cancer.
Monitor and Evaluation: Dermoscopy can monitor the progression of solar keratosis lesions over time and evaluate of the severity of keratosis.
Differentiation from other lesions: dermoscopy can show specific features such as white scales, telangiectasia, and irregular vascular structure more clearly. It helps to distinguish solar keratosis from benign lesions such as erythema, scale, ect.

What are features of dermoscopy of actinic keratosis?
When using dermoscopy to examine actinic keratosis, several features may be observed:
Structure: Brown structure-less area, ring-shaped particle structure
Distribution: The distribution of abnormal blood vessels, such as distrubution in points, lines, etc.
Pattern: Rough and irregular surface, showing a strawberry-like pattern, a fine network of thin and dark lines
Color: Color changes such as brown or red patches, regular pigmentation, especially hyper pigmentation of hair follicle openings
Other features: redness or erythema, white or yellowish scales, small black dots similar to acne (blackheads)
Dermoscopy of actinic keratosis may vary from person to person in different populations. But the most of main or key features like above listed. Dermoscopy is much helpful to distinguish actinic keratosis from other skin diseases according to the key features of dermoscopy of actinic keratosis.
The importance of timely detection and treatment of actinic keratosis
Prompt detection and treatment of solar keratosis can help protect skin health. Early treatment can prevent worsening of the condition, prevent serious complications, and reduce the risk of skin cancer. Actinic keratosis may develop into skin cancers such as squamous cell carcinoma. However,
Dermatoscopy plays a vital role in the assessment, diagnosis and treatment of solar keratosis, helping dermatologists provide personalized and effective care for patients with this common skin disorder. Dermoscopy of actinic keratosis is closely bound up the skin examinations.
Common treatment methods of actinic keratosis
By timely detection of dermoscopy of actinic keratosis lesions, appropriate treatment measures such as cryotherapy (freezing), topical drug therapy, photodynamic therapy, chemical exfoliation or surgical removal can be taken to reduce the risk of developing skin cancer. In addition, preventive measures such as sun protection (e.g. sunscreen, wearing protective clothing, avoiding peak hours of sun) and regular skin examinations can help prevent the development of new solar keratosis lesions.
Actinic keratosis is a precancerous skin lesion. if left untreated, it can not only affect the appearance of the skin, cause pain and discomfort and also increase the risk of other skin problems. Even worse, it may develop into skin cancer, such as squamous cell carcinoma. The dermoscopy of actinic keratosis plays a very important role in the early discovery and diagnosis, as well as the detection after diagnosis, and feedback on the effects of treatment. Therefore, it is vital to develop the habit of use of dermoscopy of actinic keratosis.In addition, paying more attention to sun protection and conducting regular skin examinations are also necessary in our daily life. All these measures should be used in cooperation to reduce the potential risks faced by patients, prevent the occurrence of skin cancer, and maintain the health of the skin.






















