Article
Dermoscopy of Alopecia Areata
Alopecia areata is a type of hair disease showed hair loss or baldness. It happens when immune system mistakenly attacks hair follicles, causing hair loss. Some hair fall out and then regrow and may fall out again. While some alopecia areata will never regrow hair back. It varies in kinds of complicated situation. Dermoscopy is…
Dermoscopy of Alopecia Areata: A Clinical Guide to Trichoscopy Patterns
Alopecia areata (AA) is a common autoimmune form of non-scarring hair loss characterized by sudden, patchy baldness. While clinical diagnosis is often possible, alopecia areata dermoscopy (trichoscopy) has become the standard of care for identifying subclinical disease activity and distinguishing AA from other types of non-scarring and scarring alopecias. This guide explores the pathognomonic signs of AA and how high-resolution optics facilitate accurate diagnosis and long-term management.
The Diagnostic Hallmarks: Recognizing the AA Fingerprint
In alopecia areata dermoscopy, the presence of specific follicular and hair shaft markers allows clinicians to determine the stage of the disease with high precision.
1. Exclamation Mark Hairs (The Pathognomonic Sign)
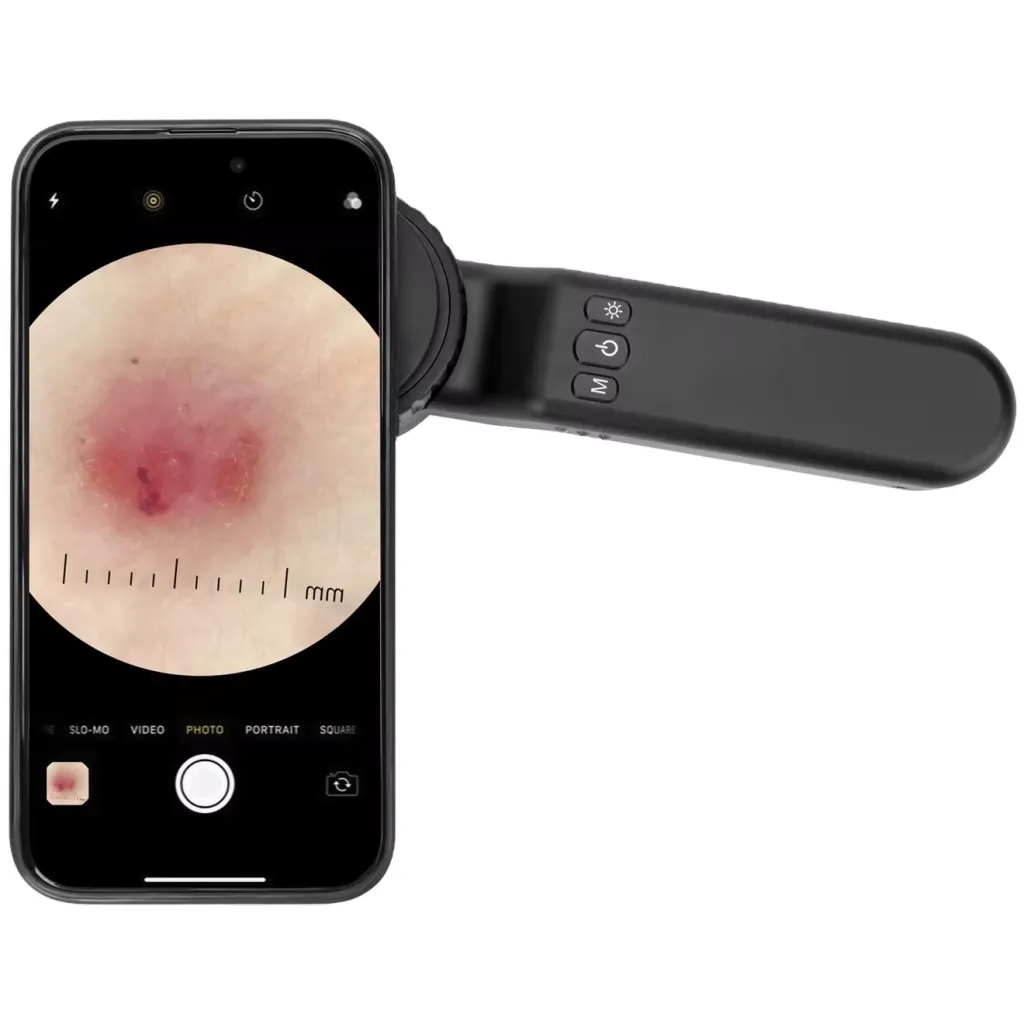
Exclamation mark hairs are the most specific sign of active AA. These are short, fractured hairs where the distal end is wider than the proximal base. Under the 10x magnification of an IBOOLO dermatoscope, these hairs appear at the periphery of expanding patches, signaling that the immune system is actively attacking the hair bulb.
2. Yellow Dots and Black Dots
Yellow dots represent follicular openings filled with keratinous debris and sebum. They are a sensitive marker for AA across all stages. Black dots, on the other hand, are the remains of hair shafts broken at the scalp level. In dermoscopy for alopecia areata, the presence of numerous black dots indicates a highly active and rapidly progressing disease phase.
3. Short Vellus Hairs (Signs of Regrowth)
Visualizing thin, pigmented, or non-pigmented upright vellus hairs within the bald patch is an encouraging sign. These "new hairs" are often the first objective evidence that the treatment is effective, long before regrowth is visible to the naked eye.
Differential Diagnosis: AA vs. Mimics
Differentiating AA from other patchy hair loss conditions is critical for appropriate therapy. Use the following comparative framework:
| Feature | Alopecia Areata (AA) | Trichotillomania | Tinea Capitis |
|---|---|---|---|
| Key Sign | Exclamation mark hairs. | Hairs of varying lengths. | Comma and corkscrew hairs. |
| Follicular Dots | Yellow and Black dots. | Black dots (fractured). | Occasional black dots. |
| Scalp Surface | Smooth, no inflammation. | Hemorrhages possible. | Scaly, erythematous. |
Assessing Disease Activity via Trichoscopy
A structured alopecia areata dermoscopy exam helps clinicians categorize the disease state: - Active Phase: Characterized by exclamation mark hairs, black dots, and "cadaverized hairs." - Chronic/Stable Phase: Predominantly yellow dots with an absence of active hair shaft fractures. - Regrowth Phase: Appearance of pigtail hairs and short vellus hairs.
Advanced Clinical Workflow with IBOOLO Optics
Achieving the clarity required for trichoscopy necessitates superior hardware. IBOOLO devices, such as the DE-4100 Pro, enhance the workflow through: - High-Resolution Lenses: Essential for identifying the delicate "tapering" of exclamation mark hairs. - Polarized Light Mode: Critical for visualizing yellow dots without surface reflection from scalp oils. - Smartphone Integration: Universal adapters allow for Sequential Digital Dermoscopy Imaging (SDDI). Clinicians can capture 4K images at baseline and 3-month intervals to objectively track hair density increase and regrowth efficacy.
Frequently Asked Questions
Can dermoscopy distinguish AA from scarring alopecia?
Yes. AA is characterized by preserved follicular openings (yellow dots), whereas scarring alopecias show ivory-white patches and a total loss of follicular ostia.
Why are yellow dots common in AA?
Yellow dots are caused by the accumulation of sebum and keratin in the follicular infundibulum when the hair shaft is absent due to the immune attack.
Is polarized light better for scalp analysis?
Polarized light is generally preferred for trichoscopy as it allows for the visualization of deeper vascular signs and follicular dots without the need for immersion fluid on the hair.
Alopecia areata is a type of hair disease showed hair loss or baldness. It happens when immune system mistakenly attacks hair follicles, causing hair loss. Some hair fall out and then regrow and may fall out again. While some alopecia areata will never regrow hair back. It varies in kinds of complicated situation. Dermoscopy is a special significant instrument to detect and diagnose alopecia areara.
What is alopecia areata?
Alopecia areata is one of the common types of hair loss. Alopecia areata most typically appearance on the scalp or beard, showing a round or oval bald patch, without hair. And alopecia areata also can happen on anywhere of the body. Alopecia areata is an autoimmune disease which caused by attack from immune system to hair follicles that form hair in skin.
What causes alopecia areate?
When immune system mistakenly attacks hair follicles, leading in alopecia areata. There are not clear reports about what exactly causes the immune attack on hair follicles, but some key factors include:
Genetic Factors: There are genetic factors in the development of alopecia areata due to it has a family tendency.
Autoimmune Factors:The immune system mistakenly targets hair follicles, resulting in hair loss.
Environmental Factors: An exotic virus or another substance happened in the body or other environmental changes may contribute to the development of alopecia areata.

Clinical features of alopecia areate
Alopecia areata usually presents as localized patchy hair loss, ranging from small round patches on the scalp to total body hair loss. It may also affect hair in other parts of the body. The typical clinical features of alopecia areata as following:
Patchy hair loss: Patchy hair loss is the most common form of presentation, with round or oval patches of hair loss and normal skin growth around the patches.
Distribution: Alopecia areata most often occurs on the scalp, but it may also occur in the beard, eyebrows, eyelashes and limbs. Complete follicular openings: The complete follicular openings are directly visible under the dermatoscope.
Positive pull test: Pulling hair will cause hair loss
Terminal hair: In bald patches, terminal hair is completely lost. Others: itching, burning or tingling, no active folliculitis and no symptoms such as erythema, desquamation or pustules around the hair follicles.
Dermatoscopic features of alopecia areata
Dermoscopy is a non-invasive aiding medical instrument that allows precise and tiny details of structures or patterns which are invisible by naked eyes. Dermoscopy of hair, also known as trichoscopy, is ideal and reliable device because it can eliminate light reflection and glare from the surface of the skin. Sometimes it is difficult to distinguish scarring alopecia from non-scarring alopecia, in which case dermoscopy can be really helpful. There are some key dermoscopic features like below:
Yellow spots: Yellow spots can be seen in both acute and chronic alopecia areata and they are yellow circular structures, usually located around the opening of the hair follicle. The presence of yellow spots may be related to inflammation and immune responses.
Black spots: Black spots is a common dermoscopic feature that indicates alopecia areata is in active state . Black spots present broken hairs at the opening of the hair follicle, usually black or brown. They may appear in the center or edges of hair loss patches.
Conical hair: This is a specific dermoscopic feature that shows tiny conical, short and spiky hair tapers gradually toward the scalp, similar to an exclamation point.
Broken hair: Broken hair are short, fractured and broken hairs usually appears in the affected area or the edges of hair loss patches.
Hypopigmentation villi: Hypopigmentation villi are hair that is sparse, short and light in color. This feature usually appears in remission of alopecia areata.

Uses of dermoscope in alopecia areata
Dermoscopy palys a crucial roles in the detection and diagnosis of alopecia areata. There are some typical uses:
1, According to dermatoscopic features of alopecia areata, dermoscopy can accurately distinguish alopecia areata from other types of hair loss, such as scarring alopecias, involutional alopecia, alopecia universalis, trichotillomania, and so on.
2, By dermoscope, skin doctors can exclude other possible causes, like fungal infection, etc.
3, Under the dermoscopy, it is clearly to evaluate the activity and severity of alopecia areata, then to make suitable treatment project
Dermoscopy for the treatment and follow up of alopecia areata
Evaluate the treatment effect: Dermoscopy can give feedback to the treatment effect of alopecia areata, So that skin doctor can analyse and evaluate if the treatment project need to be adjust or not.
Monitor relapse and detect new lesion: Dermoscopy, as a monitor, can inspect the whole process of alopecia areata, including its regrowth, relapse or new lesion.
Cooperate with treatment: By using of dermoscopy and combining with internal and external medication or other treatment methods, it greatly increase the cure effect of alopecia areata.
Notes of the use of dermoscopy in self-examination
It is no doubt that dermoscopy is very useful and reliable device in the diagnosis of alopecia areata. While, there are some notes when people use dermoscopy for self-examination.
Firstly, it is important to rightly operate a dermoscopy and carefully observe the alopecia areata in the process of the examination.
Secondly, skin doctors can compare and analyse the changes of images under dermoscopy, or images photoed by dermoscopy.
Thirdly, when a suspicious finding happened, it is necessary to ask a professional dermatologist for help.
Alopecia areata is a autoimmune skin disease. Even in some cases, hair can regrow back. But it takes undefined time. It may take 6 weeks or 1 year or more long time for hair regrowing. When hair regrow, and it may fall out again. Such situations happen time and again. And some alopecia areata represents, and it will not regrow any more. The development of alopecia areata is very complicated, so it is very important to use dermoscopy to detect and monitor alopecia areata.
No matter patients or skin doctors, all of them should know how to use dermoscopy in right ways. Especially, patients who have alopecia areata diagnosed. Pay more attention to alopecia areata and keep self-examination by dermoscopy. Any suspicious findings, keep in touch with professional skin doctors and cooperate with doctors in diagnosis and treatment.






















