Article
Dermoscopy of Bowen Disease
Bowen disease, also known as squamous cell carcinoma in situ, is a squamous cell carcinoma that occurs within the epidermis of the skin and mucous membranes. Bowen’s disease, although relatively benign in clinical presentation, is histologically characterized as carcinomatous in nature. If left untreated, the tumor cells in some cases eventually move down into the…
Clinical Guide: Mastering Bowen Disease Dermoscopy and Diagnostic Features
In the specialized field of cutaneous oncology, Bowen disease dermoscopy has emerged as a cornerstone for identifying squamous cell carcinoma in situ. Bowen disease represents a non-invasive but malignant transformation within the epidermal layer. Because it frequently mimics benign inflammatory conditions, utilizing high-resolution optical imaging is essential for early detection and preventing progression into invasive squamous cell carcinoma.
At IBOOLO, we recognize that precision diagnostics require superior optical performance. This guide explores the hallmark patterns, vascular archetypes, and clinical diagnostic strategies required for the effective management of Bowen disease.
Pathophysiological Indicators in Bowen Disease Dermoscopy
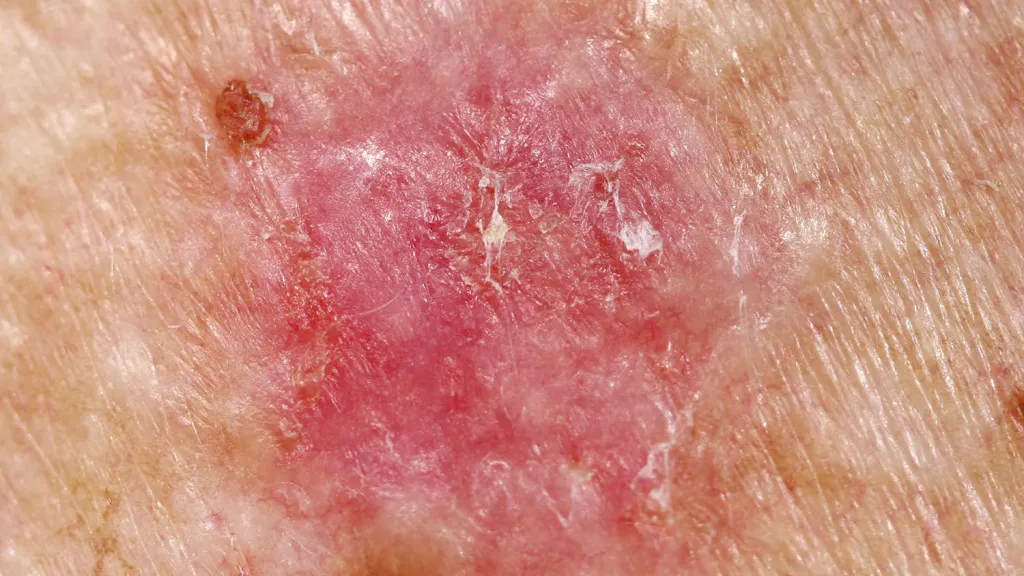
Bowen disease typically presents as a slow-growing, erythematous scaly plaque. Under the dermoscope, these biological changes manifest as structural disorganization. Advanced dermoscopic technologies allow for the visualization of subsurface hallmarks that define the degree of cellular atypia within the stratum corneum and epidermis.
Hallmark Features in Bowen Disease Dermoscopy
The clinical effectiveness of a Bowen disease dermoscopy screening depends on identifying a combination of specific morphological clues. Clinicians should focus on the following key diagnostic indicators:
- Glomerular or Coiled Vessels: These are convoluted capillaries that resemble the glomeruli of the kidney. In a Bowen disease dermoscopy exam, they often appear in clustered arrangements, providing a high degree of diagnostic specificity.
- Surface Scales: White or yellowish scales are frequently present, reflecting the abnormal keratinization of the tumor cells.
- Pigmented Features: In pigmented variants, brown-to-blue-gray dots or structureless areas may be observed, often necessitating a careful differentiation from melanoma.
- Crystalline Structures: Visible only under polarized light, these shiny white streaks represent stromal changes and are significant markers for malignancy.
Differential Diagnosis: Bowen Disease vs. Common Mimickers
The ability to differentiate Bowen disease from similar-looking lesions is the primary utility of professional dermoscopy. The following table highlights the critical differences between Bowen disease, Psoriasis, and BCC.
| Diagnostic Feature | Bowen Disease | Psoriasis | Basal Cell Carcinoma (BCC) |
|---|---|---|---|
| Vascular Pattern | Glomerular / Clustered | Regular Red Dots | Arborizing / Branching |
| Scale Distribution | Patchy / Yellow-White | Diffuse / Silvery-White | Absent / Minimal |
| Surface Quality | Erythematous Plaque | Inflamed Patches | Pearly / Translucent |
Optimizing Accuracy with IBOOLO Imaging Technology
Reliable Bowen disease dermoscopy requires an instrument that provides high resolution and specialized lighting. Polarized dermoscopy is essential for visualizing glomerular vessels and crystalline structures without the need for interface fluids, while non-polarized light is preferred for evaluating surface scales.
IBOOLO professional dermatoscopes are engineered to support both modalities, enabling clinicians to capture high-resolution images for digital documentation. By integrating these tools into the routine clinical workflow, practitioners can monitor evolving lesions and significantly improve early detection rates for squamous cell carcinoma in situ.
Mastery of Bowen disease dermoscopy features is a prerequisite for modern dermatological surveillance. By combining pattern recognition with high-performance optical tools, clinicians can ensure early detection and successful patient outcomes.
Bowen disease, also known as squamous cell carcinoma in situ, is a squamous cell carcinoma that occurs within the epidermis of the skin and mucous membranes. Bowen’s disease, although relatively benign in clinical presentation, is histologically characterized as carcinomatous in nature. If left untreated, the tumor cells in some cases eventually move down into the dermis and develop into classic squamous cell carcinoma.
Dermoscopy is a non-invasive, quick and easy test. Through dermoscopy, the doctor can observe the skin structures of Bowen’s disease, such as pigmentation, blood vessel distribution, and other features that can provide a basis for diagnosis.
Overview of Bowen Disease
Bowen’s disease is a squamous carcinoma in situ of the skin that occurs only in the cells of the stratum corneum of the skin without breaking through the basement membrane bands of the skin. It is most common in middle-aged and older adults and can occur on the skin and mucous membranes anywhere on the body, most often on the head, face, and extremities. Long-term sunlight exposure to ultraviolet radiation can damage intracellular DNA, and when DNA repair is delayed or fails, normal epithelial cells may become cancerous. The course of the disease is slow, with light or dark red papules and small patches in the early stage, which may gradually increase in size and merge into plaques of different sizes and irregular shapes, with a flat surface, and hyperkeratosis and crusting are common.
Several years after the onset of Bowen’s disease, malignant tumors of the integumentary system may develop. Therefore, Bowen’s disease should be followed up periodically after detection to observe the development of malignant tumors in the visceral system.

Dermoscopy Techniques
The optical system of a dermatoscope usually consists of multiple sets of magnifying lenses that magnify the image of the skin surface several times, making it easy to observe the structure and color changes of the skin. The dermoscopy process is relatively simple and short. However, it should be noted that the skin surface to be examined needs to be carefully cleaned before the examination, and the observation should be adjusted to the appropriate focal length.
Dermoscopy can magnify the details of the skin of patients with Bowen’s disease and help doctors observe the characteristic manifestations of Bowen’s disease-like papulopapular disorder, such as the size, shape, and color of the macular rash, as well as the covering of greasy scabs and scales. This helps doctors to better treat their patients.
What does Bowen Skin Cancer Look Like?
Bowen skin cancer lesions are initially red spots, round or oval, gradually expanding and irregular in shape. The surface is often accompanied by keratinized scales, and the boundary of the lesion is clear, which may be slightly elevated, and there are generally no self-conscious symptoms. Chronic eczema and Bowen’s disease have some similarity in the morphology of the lesions, manifested as erythema of the skin, accompanied by itching, easy to recur. However, chronic eczema usually has obvious itching symptoms and a longer course.

Specific Dermoscopic Features of Pigmented Bowen’s Disease
The dermoscopy of Bowen disease is often characterized by clustered distributions of punctate, coiled blood vessels. This vascular structure is highly specific in Bowen’s disease and is one of the most important clues to the diagnosis of the disease. The surface of the lesions in Bowen’s disease is usually accompanied by scales, which are caused by hyperkeratosis of the epidermis. Pigmented Bowen’s disease is relatively rare, and its dermatoscopic features, in addition to the typical manifestations described above, are characterized by the following specific features: brown keratotic structureless area, homogenous area of different shades and brown-to-blue-gray dots/ peppering.
Differential Diagnosis of Bowen Disease
Bowen disease usually presents as an intraepidermal abnormality, whereas superficial basal cell carcinoma often occurs on the trunk, especially the back and chest. Whereas malignant melanoma is a pigmented tumor, Bowen’s disease does not necessarily contain pigment.Pigmented Bowen’s disease is rare. It is commonly described in dark skin individuals and on the sun-protected areas.
Dermoscopy not only magnifies the lesions, but also clearly shows the pigmentation and blood vessels of the skin. Different skin diseases will present different skin patterns, and dermoscopy can be very helpful in differentiating between them.
Clinical Case Studies
Clinically, Bowen’s disease usually presents as well-defined, irregularly shaped light-red or dark-red papules or plaques with a few scales or crusts on the surface, with no obvious characteristic manifestations, which can be easily confused with other diseases.
The vascular structure of Bowen’s disease is usually characterized by dots, clumps or lines in dermoscopy, and glomerular blood vessels are also one of the classic features. And structureless pigmentation is often seen in dermoscopy.
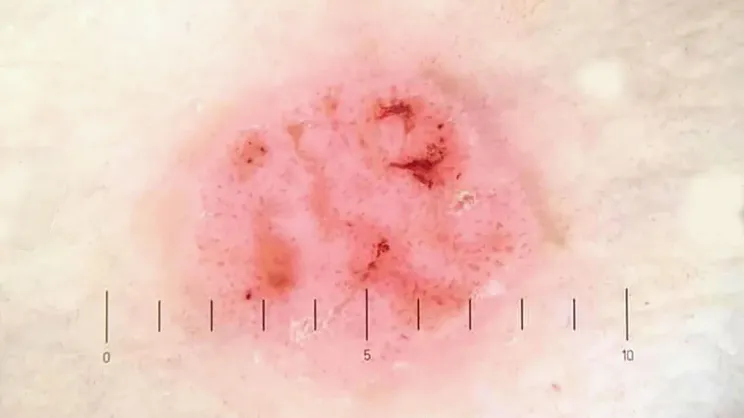
Dermoscopy is capable of observing fine structures that cannot be seen by the naked eye, such as glomerulonephric blood vessels and structureless pigmentation, etc. These features are of great significance in the diagnosis of Bowen’s disease. Bowen’s disease is easily confused with psoriasis, eczema and solar keratosis. Dermoscopy can show the specific dermoscopic features of different diseases, which can help doctors to make differential diagnosis.
Treatment and Management of Bowen Disease
Surgical removal of the Bowen’s disease tissue completely is one of the common treatments for larger skin lesions. Bowen’s disease can also be cured by rapid freezing of the damaged area by a medical professional using liquid nitrogen, which causes necrosis of the diseased tissue through extremely low temperatures. Photodynamic therapy is another commonly used treatment, which is usually well tolerated, has mild side effects, and is cosmetically effective.
Once cured, patients with Bowen’s disease should avoid sun exposure and eat a light diet while maintaining a good state of mind. And doctors consider following up each case of Bowen’s disease depending on the size of the lesions, treatment modality and immunosuppression.
Prevention and Screening for Bowen Disease
When outdoors, try to avoid prolonged exposure to sunlight during periods of intense UV light. Regular skin examinations can help detect Bowen’s disease early. Through examination by a medical professional, abnormal changes in the skin, such as dark red, brownish-red or brown patches, can be detected in time for further diagnosis and treatment.
In the early detection of Bowen’s disease, dermoscopy, as a non-invasive, quick and easy method of diagnosing skin disorders, can quickly help doctors to determine how far the lesions have progressed.
Recommended reading
China Manufacturer & Factory Specializing in Professional Dermoscopy Models - IBOOLO
Through engineering mastery nurtured over a decade, our China manufacturer & factory produces Professional dermoscopy devices combining sturdy builds and unmatched optics for flexible precision skin analysis.
Dermoscopy of Lentigo Maligna – IBOOLO
Lentigo maligna is a form of potentially serious skin cancer, and it is a early stage of lentigo maligna melanoma. Malignant cells of lentigo maligna usually occur in the epidermal layer of the skin. When its malignant cells invade into the dermis or deeper of the skin, then lentigo maligna transforms into lentigo malignant melanoma....
Buy the best dermatoscopes for skin screening and analysis - IBOOLO
IBOOLO offers the best professional dermatoscopes available for purchase buy online. Shop a range of digital dermatoscopes for dermoscopy, mole screening, clinical analyses, and more.






















