Article
Dermoscopy of Lichen Planopilaris
The clinical significance of lichen planopilaris is mainly reflected in the impact on patients’ quality of life. It can lead to patchy or diffuse baldness of the scalp, which not only affects the patient’s appearance, but may also have a negative impact on the patient’s mental health. Early and accurate diagnosis of lichen planopilaris can…
The clinical significance of lichen planopilaris is mainly reflected in the impact on patients’ quality of life. It can lead to patchy or diffuse baldness of the scalp, which not only affects the patient’s appearance, but may also have a negative impact on the patient’s mental health. Early and accurate diagnosis of lichen planopilaris can help to take timely treatment measures to slow down the progression of the disease and reduce the area of hair loss. Dermoscopy can clearly observe the characteristic lesions such as erythema, desquamation, follicular hyperkeratosis, and clustered spiny follicular papules around the hair follicles of patients with lichen planopilaris, which can provide an intuitive and accurate basis for the diagnosis of lichen planopilaris.
What Is Lichen Planopilaris?
Lichen Planopilaris, also known as trichophytic lichen planus, is a form of primary lymphocytic scarring alopecia that mainly effects the scalp. The exact cause of tinea versicolor is unknown, but it may be the result of a variety of issues including immune system abnormalities, genetic factors, fungus on your skin and emotional stress.
Lichen planopilaris mainly shows patchy alopecia or diffuse hair loss on the scalp, with active lesions at the margins of bald patches including perifollicular erythema and desquamation with follicular hyperkeratosis. Associated symptoms include pruritus and pain, which are various in severity.

Epidemiology and Classification of Lichen Planopilaris
The incidence of lichen planopilaris is relatively low worldwide, with a reported prevalence of about 1%. More often than men followed by women, this disease is present in the age bracket of 30 to 70 years old. Lichen planopilaris can be classified into the following types or subtypes based on their clinical presentation and pathologic features: classic lichen planopilaris, frontal fibrosing alopecia, and Graham-Little-Piccardi-Lasseur syndrome.
Dermoscopy in the Diagnosis of Lichen Planopilaris
Dermoscopy is an optically based dermatologic diagnostic tool that focuses on magnifying the surface of the skin through the use of an optical magnification system so that the physician can see the texture and details of the skin surface more clearly. Dermoscopy also improves the contrast and clarity of the image through the use of optical filters and color filters.
Lichen planopilaris is a chronic inflammatory skin disease that primarily affects the hair follicles of the scalp. It has some characteristic manifestations under dermoscopy, such as erythema around the hair follicles, punctate hemorrhage at the mouth of the hair follicles, and atrophy of the scalp, which can help doctors to make a differential diagnosis. Meanwhile, dermoscopy, as a non-invasive means of examination, can observe the characteristics of lesions without damaging the skin, reducing the pain and discomfort of patients.
Prior to dermoscopy, patients should avoid applying medications or cosmetics to the skin surface prior to the examination, and especially avoid applying sunscreen and other substances that may block light from the imaging. During the examination, the patient should try to cooperate with the examiner and assume the proper position so that the skin lesions can be fully exposed. After the examination, patients need to pay attention to keep the local skin clean and dry, and avoid scratching the affected area, so as not to cause skin infection.

Dermoscopic Features of Lichen Planopilaris
Absence of follicular openings: In advanced lesions of Lichen Planopilaris, the follicular openings may be completely absent, resulting in visible patches of alopecia on the scalp.
Perifollicular erythema: In active lesions, perifollicular erythema can be observed, and these are usually accompanied by signs of desquamation and follicular hyperkeratosis.
Classic white and blue-gray spots: On dermoscopic examination, Lichen Planopilaris may exhibit irregular white spots between hair follicles and bluish-gray spots around hair follicles.
White scarred areas: Areas of white scarring usually form as a result of complete loss of hair follicles and fibrosis of the skin, and are typical of advanced stages of lichen planus.
Milky red areas: On dermoscopy, localized congestion or vasodilatation due to an inflammatory response may be observed, and these usually appear as red or pink areas.
Lichen Planopilaris and Other Alopecia Areata Disorders
Lichen Planopilaris differs significantly from other alopecia areata disorders (e.g., discoid lupus, frontal fibrotic alopecia) in terms of dermoscopic features. Dermoscopy is able to magnify the area of skin lesions, details of skin surface microstructure, hair shaft morphology, and capillaries, providing visual evidence for differential diagnosis.
Lichen Planopilaris: Dermoscopy reveals a marked inflammatory reaction around the hair follicle in the form of erythema, edema, or desquamation, and these changes are distributed around the hair follicle in a ring or target-shaped pattern. The follicular opening may become inconspicuous or disappear completely, and sometimes the follicular opening can be seen to be blocked by keratin plugs.
Discoid Lupus: The follicular opening is seen as a distinct red spot, which is often surrounded by a white halo. In advanced lesions, due to fibrosis of the dermis, white structureless areas are seen dermoscopically; these areas correspond to scar tissue in the dermis.
Frontal Fibrotic Alopecia: There is a marked reduction in the number of hair follicles in the frontal region, especially the reduction of coarse hairs. Erythema around the hair follicles may be present in the area of hair loss. The forehead skin may become smooth and tight, losing normal skin texture and elasticity.
Case Study
Clinical and dermoscopic images of lichen planopilaris are shown below respectively.

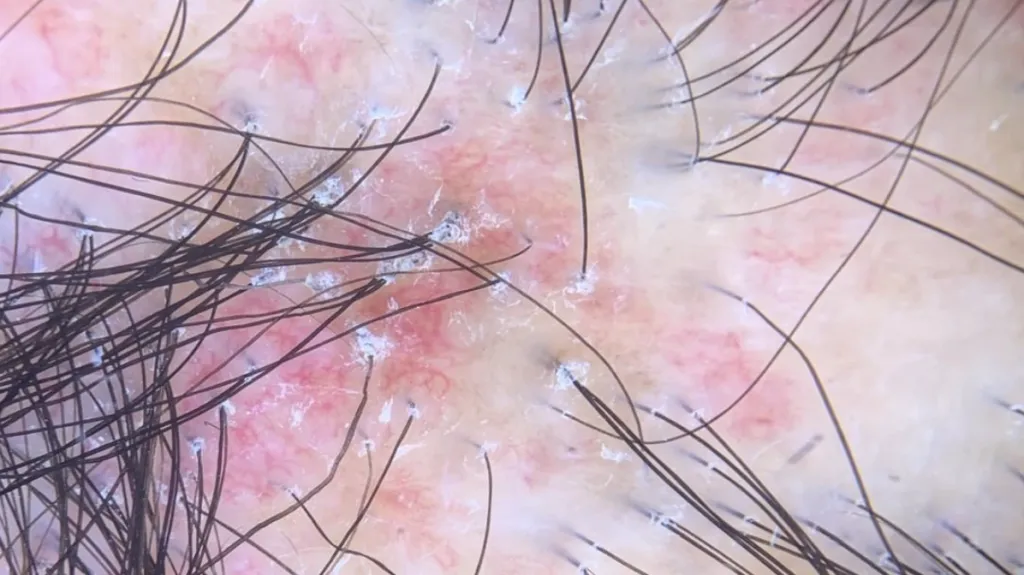
By comparing the clinical and dermoscopic images of lichen planopilaris we can see that the dermoscopic images show the fine structure of the follicular units more clearly. The dermoscopic image shows scales around the hair follicle as well as a hair tube pattern, and keratinous plugs are visible at the follicular openings, which are due to hyperkeratosis and blockage of the follicular openings with large amounts of keratinized material. Blue-gray spots around the hair follicles, forming target-like pigmentation, are typical features of lichen planopilaris, and the doctor can make a preliminary judgment of the disease based on them.
Dermoscopy is an important tool for initial diagnosis, but pathologic examination remains the gold standard for diagnosis. For patients with suspected LPP, pathologic examination should be performed as early as possible to confirm the diagnosis and reduce the possibility of misdiagnos.
Treatment and Management of Lichen Planopilaris
The treatment of lichen planopilaris mainly includes medication, physical therapy and surgery. Patients should eat more fresh vegetables, ensure enough sleep and face the disease with an optimistic attitude to help the disease recover. After treatment, doctors should closely observe whether the patient’s symptoms are reduced. According to the improvement of the patient’s rash, it will be categorized into four grades for evaluation: cured, obvious effect, effective and ineffective.
Lichen planopilaris is a chronic disease that requires long-term management and treatment. Patients should take the medication on time as prescribed by the doctor and should not stop taking the medication or change the dosage at will. Health education should be strengthened to improve patients’ knowledge of the disease and self-management ability.
Lichen Planopilaris Dermoscopy for Accurate Diagnosis - IBOOLO
IBOOLO dermoscopy enhances lichen planopilaris diagnosis. Learn key features, differential diagnosis, and treatment options. Improve early detection and patient care.
Lichen Planopilaris Dermoscopy: Precision Diagnosis with IBOOLO
Lichen planopilaris dermoscopy reveals critical features like peripilar scales and follicular ghosts, enabling early detection and differentiation from alopecia areata. IBOOLO’s advanced dermoscopes enhance diagnostic accuracy, reduce unnecessary biopsies, and support long-term monitoring. This article explores key dermoscopic signals, differentiation techniques, and follow-up strategies for lichen planopilaris.
What is Lichen Planopilaris?
Lichen planopilaris (LPP), a chronic inflammatory hair disorder, primarily affects middle-aged women, often leading to permanent hair loss. Dubbed the "baldness curse" due to its progressive nature, early identification is crucial. Lichen planopilaris dermoscopy provides a non-invasive method to detect subtle follicular changes, aiding timely clinical decisions.
- Appearance: Patchy hair loss, scalp redness, or itching.
- Common Sites: Scalp crown, hairline, or occipital area.
- Risk Factors: Autoimmune conditions, stress, or genetics.
Role of Dermoscopy in Lichen Planopilaris Diagnosis
Dermoscopy lichen planopilaris uses high-magnification imaging to reveal microstructural details invisible to the naked eye. IBOOLO’s dermoscopes, with polarized light and digital capture, enhance visualization of lichen planopilaris dermoscopy features, ensuring accurate early detection and differentiation from other hair loss conditions.
Three Key Dermoscopic Signals
Lichen planopilaris dermoscopy highlights three hallmark signals for early identification:
- Peripilar Scales and Erythema: White scales encircling hair follicles, often with redness, indicating active inflammation.
- Follicular Keratotic Plugs: White or yellow plugs blocking follicle openings, marking follicular damage.
- Progressive Follicular Loss: Gradual disappearance of follicles, replaced by ivory-white scar-like areas.
These signals, observed through dermoscopy lichen planopilaris, guide clinicians but require professional interpretation to confirm suspicion.
Why These Signals Appear
Peripilar scales in lichen planopilaris dermoscopy reflect inflammatory activity around follicles, while keratotic plugs indicate follicular obstruction. Progressive follicular loss, seen as scar-like areas, signifies irreversible damage due to chronic inflammation, a hallmark of LPP’s scarring process.
How Dermoscopy Works for Lichen Planopilaris
IBOOLO’s dermoscopy technology employs 10x–100x magnification and polarized light to eliminate surface glare, revealing lichen planopilaris’s follicular details. Digital imaging supports documentation, making dermoscopy lichen planopilaris ideal for non-invasive diagnosis and monitoring.
Step-by-Step Dermoscopic Examination
To identify lichen planopilaris on dermoscopy, clinicians follow a systematic process:
- History Review: Assess hair loss onset, symptoms, and autoimmune history.
- Scalp Preparation: Clean the area and apply a gel interface for clarity.
- Scalp Scan: Examine hairline, crown, and occipital areas for follicular changes.
- Feature Identification: Focus on scales, plugs, and follicular loss using IBOOLO’s dermoscope.
- Image Capture: Record findings for diagnosis and future comparison.
Professional interpretation of lichen planopilaris dermoscopy findings is essential for accurate diagnosis.
The Follicular Ghost and Scale Ring in Lichen Planopilaris
In lichen planopilaris dermoscopy, "follicular ghosts" (faint, hairless follicle remnants) and "scale rings" (white scales encircling follicles) are highly characteristic.
Evaluating These Features
- Scalp Overview: Assess follicular density and distribution.
- Follicular Focus: Identify scale rings and keratotic plugs around follicles.
- Ghost Detection: Note faint, hairless follicle remnants indicating loss.
- Pattern Analysis: Confirm the presence of both features as dominant patterns.
These features, unique to dermoscopy lichen planopilaris, reflect inflammation and scarring but require professional interpretation.
Differentiating Lichen Planopilaris from Alopecia Areata
Lichen planopilaris dermoscopy is vital for distinguishing LPP from alopecia areata, a common misdiagnosis due to similar patchy hair loss.
Key Dermoscopic Differences
- Lichen Planopilaris: Peripilar scales, keratotic plugs, follicular loss, and ivory-white scarring.
- Alopecia Areata: Exclamation mark hairs, yellow dots, black dots, and no scarring.
Dermoscopy lichen planopilaris reveals scarring and inflammatory patterns, unlike the non-scarring, hair-specific features of alopecia areata. Professional evaluation is critical to avoid misdiagnosis.
Monitoring Lichen Planopilaris with Dermoscopy
Lichen planopilaris may recur due to its chronic inflammatory nature. Lichen planopilaris dermoscopy enables non-invasive tracking of disease activity and treatment response.
Features Monitored During Follow-Up
- Inflammatory Signs: Extent of peripilar erythema and scale distribution.
- Follicular Status: Changes in follicle clarity, hair density, or quality.
- Disease Progression: New keratotic plugs or expanding follicular loss.
- Treatment Response: Reduction in inflammation or stabilization of follicular loss.
Dermoscopy lichen planopilaris provides objective records for comparison, but professional interpretation is essential.
Benefits of Long-Term Dermoscopic Monitoring
- Baseline Imaging: Establishes reference images for tracking changes.
- Early Recurrence Detection: Identifies subclinical inflammatory signs.
- Treatment Evaluation: Assesses intervention efficacy.
- Patient Education: Visualizes disease progression for better understanding.
Dermoscopy vs. Biopsy for Lichen Planopilaris
Lichen planopilaris dermoscopy enhances screening but cannot replace biopsy for definitive diagnosis.
Advantages of Dermoscopy
- Non-Invasive: Avoids pain and scarring, ideal for screening.
- Rapid Insights: Reveals follicular details instantly.
- Monitoring Efficiency: Tracks changes without invasive procedures.
Dermoscopy lichen planopilaris supports early detection and reduces unnecessary biopsies in typical cases.
When Biopsy is Necessary
- Atypical Features: Non-classic patterns or overlap with other conditions.
- Disease Progression: Rapid hair loss or new symptoms.
- Clinical Uncertainty: When dermoscopy cannot confirm LPP.
Biopsy remains the gold standard, guided by lichen planopilaris dermoscopy findings.
Enhancing Lichen Planopilaris Care with IBOOLO
IBOOLO’s dermoscopy solutions optimize lichen planopilaris management:
- Advanced Dermoscopes: High-resolution imaging with polarized light.
- Clinician Training: Programs to master LPP-specific features.
- Patient Education: Informs patients about screening benefits.
- AI Integration: Enhances accuracy with automated pattern analysis.
Lichen planopilaris dermoscopy, powered by IBOOLO’s technology, transforms the diagnosis and monitoring of this scarring alopecia. By revealing peripilar scales, follicular ghosts, and progressive loss, it distinguishes LPP from alopecia areata and supports effective follow-up. While a vital screening tool, dermoscopy lichen planopilaris requires professional interpretation to complement clinical judgment, ensuring optimal patient outcomes.






















