Article
Dermoscopy of Malenoma
What is malignant melanoma?Malignant melanoma is a serious skin cancer that starts in melanocytes. It is also known as cutaneous melanoma. This skin cancer is much dangerous due to its rapidly spread to other organs if it is not controlled at an early stage.Melanoma can appear in anywhere on the skin, but for people with…
Malignant Melanoma Dermoscopy: Clinical Diagnostic Patterns and Guide
In contemporary dermatology, the accuracy of malignant melanoma dermoscopy has become the benchmark for non-invasive clinical excellence. As the most aggressive form of skin cancer, melanoma requires a diagnostic approach that transcends simple visual inspection. By utilizing high-resolution optical systems, clinicians can visualize the intricate micro-architecture of lesions, leading to earlier intervention and significantly improved patient survival rates.
Mastering melanoma dermoscopy involves a sophisticated understanding of morphological disorganization. While benign nevi typically exhibit symmetrical patterns and uniform structures, malignant lesions are characterized by a breakdown in cellular organization that manifests through specific dermoscopic clues.
Hallmark Patterns in Malignant Melanoma Dermoscopy
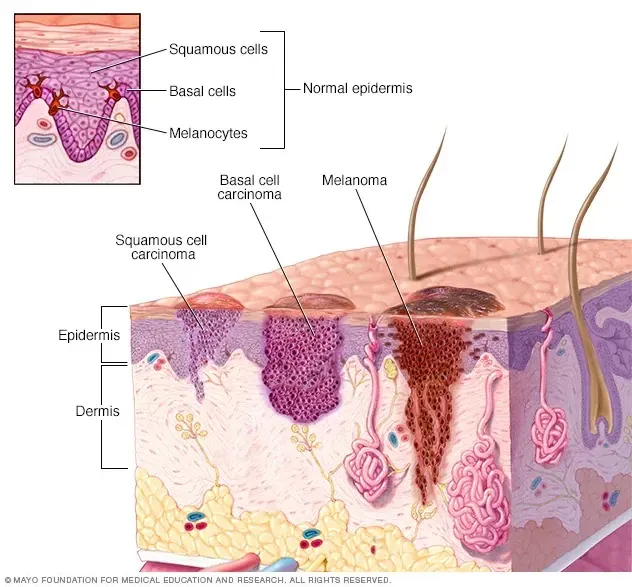
The identification of malignant melanoma dermoscopy features is based on the recognition of several key diagnostic criteria. These features are direct reflections of the underlying histopathological changes occurring within the epidermis and dermis.
1. Atypical Pigment Networks and Structural Chaos
The pigment network is often the first area of focus. In malignant melanoma dermoscopy, this network becomes chaotic. Clinicians look for lines that vary significantly in thickness and spacing, creating an irregular lattice. A hallmark red flag is the abrupt termination of the network at the periphery, where the pigment stops suddenly rather than fading into the surrounding skin.
2. Regression Structures: The Blue-White Veil
A blue-white veil is one of the most specific indicators in melanoma dermoscopy. This hazy, gray-blue discoloration represents deep dermal melanin or focal orthokeratosis. Its presence within a suspicious lesion significantly increases the likelihood of malignancy and serves as a primary indicator for surgical biopsy.
3. Vascular Morphology and Neoangiogenesis
Tumor growth is accompanied by abnormal vascularization. Through malignant melanoma dermoscopy, these vessels appear disorganized. Patterns to observe include dotted vessels chaotically distributed, linear-irregular (serpentine) vessels, and polymorphous patterns where multiple vessel types exist within the same lesion.
Clinical Comparison: Benign Nevus vs. Malignant Melanoma
The primary value of melanoma dermoscopy lies in its power of differentiation. The following table summarizes the key structural differences that guide clinical decision-making.
| Diagnostic Feature | Benign Nevus (Mole) | Malignant Melanoma |
|---|---|---|
| Structural Symmetry | High (Symmetrical in two axes) | Low (Asymmetric & Disorganized) |
| Pigment Network | Uniform, Fades at Periphery | Irregular, Abrupt Termination |
| Vascular Pattern | Typically Absent or Regular | Atypical, Linear-Irregular |
| Color Distribution | 1-2 Uniform Colors | Multiple (3+) Colors |
Optimizing Melanoma Detection with Precision Optics
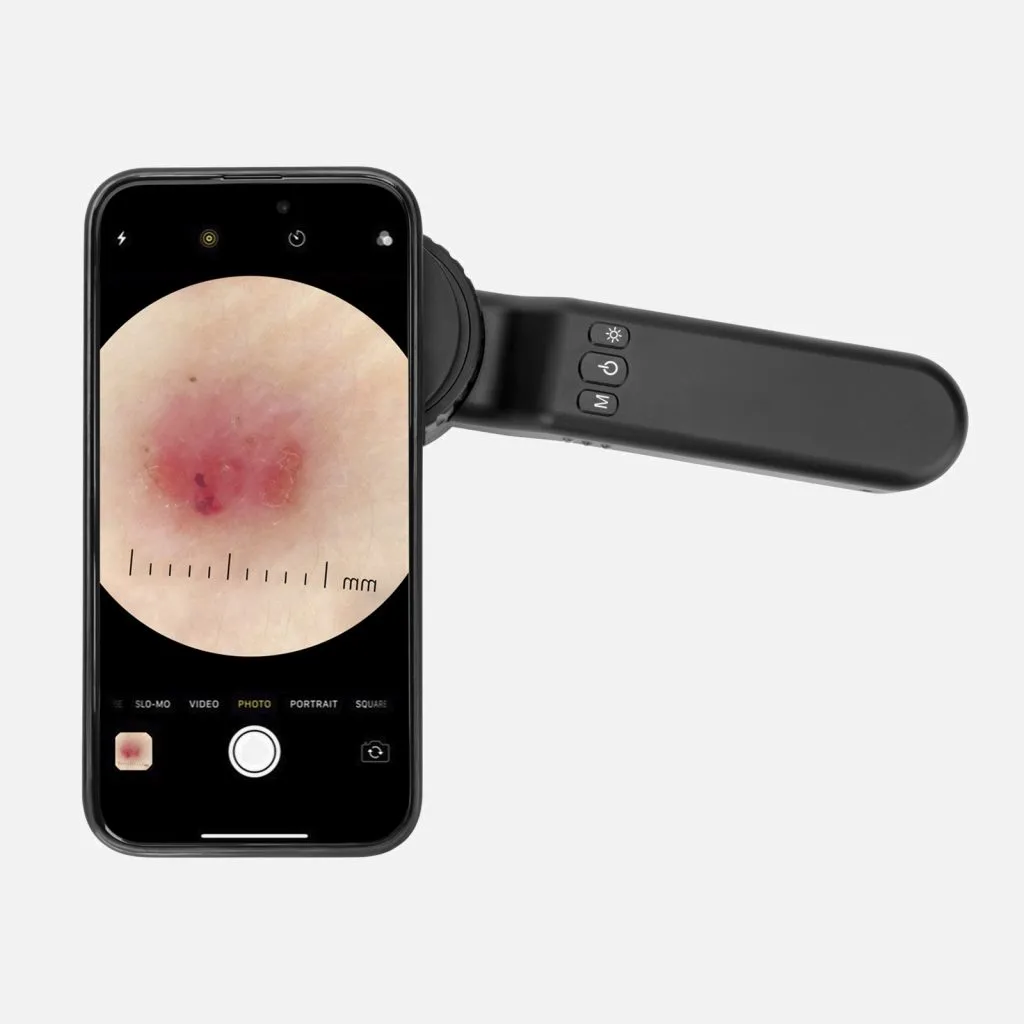
The effectiveness of melanoma dermoscopy is fundamentally tied to the quality of the instrument. High-resolution imaging provided by IBOOLO professional dermatoscopes allows for the visualization of fine streaks, pseudopods, and peripheral dots that might be missed by lower-quality lenses.
By utilizing cross-polarization technology, our devices eliminate surface glare without the need for immersion oils, facilitating a faster and more comfortable workflow. The integration of smartphone compatibility further enables sequential digital dermoscopy imaging, a critical technique for monitoring evolving lesions over time and improving diagnostic sensitivity for early-stage melanoma.
The Clinical Significance of Early Diagnosis
Evidence shows that utilizing dermoscopy can improve melanoma diagnostic accuracy by up to 27% compared to naked-eye examinations. For localized melanoma (Stage 0 to II), early identification leads to a five-year survival rate of approximately 98%. However, this rate decreases significantly as the tumor progresses to advanced stages. This statistical reality underscores the importance of integrating malignant melanoma dermoscopy into routine skin health screenings.
Malignant melanoma dermoscopy is a life-saving protocol that requires a blend of clinical expertise and high-performance technology. At IBOOLO, we are dedicated to providing the optical precision necessary for dermatologists to identify critical markers with clarity and confidence.
Recommended reading
China Manufacturer & Factory Specializing in Professional Dermoscopy Models - IBOOLO
Through engineering mastery nurtured over a decade, our China manufacturer & factory produces Professional dermoscopy devices combining sturdy builds and unmatched optics for flexible precision skin analysis.
Premier China Products Supply Produces High Quality Dermatoscopio Precios for Less - IBOOLO
As a leader among China high quality dermatoscopio precio products supplys, over 11+ years we have perfected durable, optically-superior models designed and assembled by our experienced staff.
Premier China Manufacturer & Factory Supplies Affordable Polarized Dermoscopys - IBOOLO
Through streamlined China production processes, our manufacturer & factory delivers feature-rich yet affordable polarized dermoscopys designed for ergonomics, accuracy and reliable sharpness when analyzing skin.
What is malignant melanoma?
Malignant melanoma is a serious skin cancer that starts in melanocytes. It is also known as cutaneous melanoma. This skin cancer is much dangerous due to its rapidly spread to other organs if it is not controlled at an early stage.
Melanoma can appear in anywhere on the skin, but for people with lighter skin, melanoma is more likely to start on the chest and back in men and on the legs in women. The arms, face and neck are other common areas both in men and women. People with darker skin have a lower risk of developing melanoma in these more common areas. Melanoma even can happen in the eyes, while it is rarely to form inside body, like in throat or nose.
What is the cause of melanoma?
The cause of all melanomas is not exactly clear. But melanomas risk increase with exposure to ultraviolet light. Ultraviolet light, also known as UV, comes from sun or solariums. UV radiation can damage the DNA in skin cells, causing mutations that cause the cells to grow uncontrollably and form cancerous tumors.
Melanoma commonly happens especially in tanning, and sunburn during childhood. So it is helpful to reduce the risk of malignant melanoma by limiting the exposure to UV light.
Common high risk groups
The common high risk groups include: a previous melanoma comes back, a history of the sunburns, a family history of melanoma, fair skin or red hair, having many moles or atypical moles, a weakened immune system and so on.
The risk of melanoma appears to be increasing for people under 40, especially women. It is important to understand the high incidence of melanoma in people to help to prevent it. If people find a suspected person, then he should seek medical attention as soon as possible. Melanoma can be successfully treated when it is caught in early stage.
Symptoms of melanoma
There are some common signs and symptoms of melanoma including the following characteristics:
Asymmetry: one half of a mole or birthmark does not match the other half.
Size: Melanomas feature in larger size than normal moles, often exceeding 6mm in diameter.
Color: Melanomas may display different or multiple colors or shades, like brown,black,pink,red,blue, white even mixed color.
Border: melanoma may has irregular, scalloped, notched, or blurred borders.
Pain: Some melanomas may be painful or tender to the touch. Sometimes the spot will bleed and ooze fluid.



The appearance of new and atypical spots on the skin is the most important warning sign of melanoma. And other important warning sign is the existing spots have changed in color, size and shape. However, there may be one or two unusual characteristics of melanoma. Atypical changes on skin should be pay more attention to.
Survival rates for malignant melanoma
If diagnosed and treated early, malignant melanoma has a high cure rate, and the five-year survival rate for localized melanoma is about 98%. It includes the stage 0, stage I and stage II of malignant melanoma.
If it is not founded in the early stage, and it reaches to stage III of regional melanoma , the survival rate of malignant melanoma is about 63%.
However, if malignant melanoma is not treated until it has reached a more advanced stage and has spread to other parts of the body, such as the liver, lungs or brain is more serious and challenging to treat and has a lower survival rates.The five-year survival rate for stage IV melanoma is about 22%.
No matter how, use a dermoscopy to detect the atypical spots is necessary in case of any chance for evolution of malignant melanoma. Under the dermoscopy, dermatologists can detect and diagnose malignant melanoma much easily and accurately.
Identify the characteristics of malignant melanoma by using dermoscopy
Under the dermoscopy, it is clearly to display the features of malignant melanoma. Such as, by using dermoscopy, malignant melanoma usually clearly shows Irregular edges or borders and multiple colors. And malignant melanoma commonly appears in abnormal pigment distribution and structure, or atypical vascular distribution. Special signs such as granular areas and small blue and white papules may occur. Dermoscopy can precisely distinguish the points of malignant melanoma from benign lesions such as nevus.
Dermoscopy in the diagnosis of malignant melanoma
Dermoscopy is a dependable and aiding medical technique by skin doctors to detect the melanoma. Dermoscopy combines a powerful lighting system and high quality magnify lens to enhance the view of deeper skin and some hard-to-reach locations by naked eyes. The whole process of skin examination under dermoscopy without any side effective or adverse reactions. Dermoscopy can assist professional doctors to make early diagnosis of malignant melanoma without unnecessary biopsies and surgeries. Dermoscopy helps skin doctors to determine the clinical stage of the mass. What’s more, during the whole process of detection or treatment, as a monitor, dermoscopy can observe the progression of lesions. Dermoscopy greatly helps skin doctors to evaluate the effectiveness of surgery or other treatment of malignant melanoma.
Dermoscopy in public self-examination
Dermoscopy is usually designed to a small electric device which is convenient to handheld or easy to take photo by compatible with phones and tablets. Dermoscopy gains a very popularity both in hospital and in home. Dermoscopy can easily identify the malignant melanoma in professional hands. There are some main points when people use dermoscopy in public self-examination.

Firstly, correct operation and usage is necessary.
Secondly, during the use of dermoscopy, it needs to keep precautions and observations.
Thirdly, as soon as suspicious lesions are detected by dermoscopy, then it needs to seek medical treatment promptly.
Fourthly, people should cooperate with professional doctors for diagnosis and treatment after self-examination by dermoscopy if any atypical lesions founded.
Skin health is very significant to every one. Detection of malignant melanoma is really important, especially there being negligence in its early stage. With the help of dermoscopy, it increases much more confidence for dermatologists to diagnose and treat malignant melanoma and other skin diseases. In addition, more and more people use dermoscopy to examine skin conditions. Especially, high risk groups of malignant melanoma should even more often use dermoscopy for regular self-examination.






















