Article
Dermoscopy of Nodular Melanoma
Nodular melanoma, as the second most common type of melanoma, makes up around 15 percent to 30 percent of all melanoma cases each year as reported. It is very aggressive due to its faster speed of spread than other types of diseases, especially under the skin where are invisible. High incidence rate, fast growing speed…
Nodular melanoma, as the second most common type of melanoma, makes up around 15 percent to 30 percent of all melanoma cases each year as reported. It is very aggressive due to its faster speed of spread than other types of diseases, especially under the skin where are invisible. High incidence rate, fast growing speed and hidden location bring more difficult to detect and diagnose nodular melanoma. Nodular melanoma causes around 50% of death rate in melanoma-related diseases. But if detected and treated early, there is a great rate to cure it by professional doctors. So it is special crucial to use a dermoscopy to diagnose nodular melanoma in its early stage.
What is nodular melanoma?
Nodular melanoma is a subtype of melanoma. It usually appears as a firm, discolored bump or node that similar to blood blister above the skin, can be on any part of the body, typically in arms, legs, and trunk.Nodular melanoma is famous as its fast rapid of vertical growing that means it grows quickly in thickness other than in diameter. This is the reason that nodular melanoma recognized as a dangerous and aggressive skin cancer.
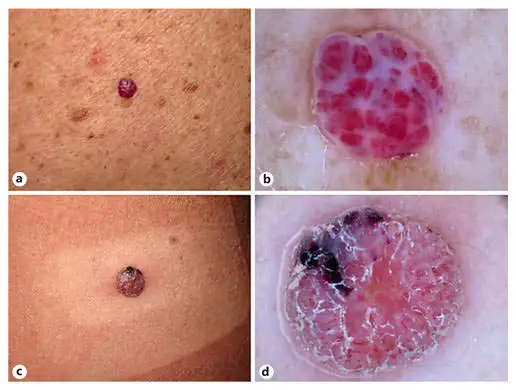
What does nodular melanoma look like?
Nodular melanoma usually presents as a round black bump or skin lesion. It looks like a mole, a blood blister, an insect bite, or a skin acne. That’s why people often mistake them for other something other than skin cancer at first. Nodular may also be blue, grey, red, white, pink or brown. Unlike other types of melanomas, nodular melanomas usually have uniform boundaries, symmetrical structure, with the papules rising above the surrounding skin. Symptoms of nodular melanoma usually include itching, tingling, bleeding, and exudation.

What causes nodular melanoma?
As we all know, liking other factors for melanoma, overexposure to ultraviolet light is also the biggest risk for forming nodular melanoma, especially over sunburns. Except for that, there are several other factors which may cause nodular melanoma, such as: genetic mutation factors, low immune systems, a family history of melanoma, age and gender( the older and man are more risk of nodular melanoma than youth and women), environmental factors, lifestyle factors and so on.
Basic Science of dermoscopy
Dermoscopy is a helpful and valuable device which built in magnification and illumination systems. It allows an enhanced visualization of the surface and subsurface structures of the skin by the basic science of dermoscopy of combining the optical system and physical system. Regarding optical system, dermoscopy usually utilize its cross polarization and non-polarization which present particular dermoscopic features in prominence. Especially it can observe very clear and precise images of structures, patterns and pigment network which are invisible by naked eyes.
Some dermoscopy are designed as a handheld tool which can be hold by skin doctors to observe the skin lesions directly, and also can be used to capture the image for later analysis and comparison. Some advanced dermoscopy are connected with computer software by USB port, detecting and analyzing skin diseases according to dermoscopic features intelligently and effectively.
Dermoscopic features of nodular melanoma
Most melanomas are according to the well-know ABCDE rules of melanoma. But It brings challenge to diagnose nodular melanoma due to its often lacking of these rules. While several typical dermoscopic features of nodular melanoma helping differentiate it from other skin cancers, such as:
Black-blue area or black-blue veil
Atypical vascular patterns
Homogeneous disorganized patterns
Homogeneous blue-black pigmented structure-less areas
Crystalline structures(seen only with polarized light of dermoscopy)
Multiple colors (often more than 3, usually 5~6 colors)
Combination of blue(located in the mid-deep dermis) and black(located in the epidermis)
Combination of polymorphous vessels and milky-red globules/areas
Asymmetrical pigmentation but symmetrical shapes
What diseases can be misdiagnosed as nodular melanoma?
Nodular melanoma is characterized as a hard, discolored bump or node that similar to blood blister above the skin. Due to its appearances are similarities with benign and malignant lesions, it challenging to be detected and diagnosed when associated with such skin diseases, like dermatofibroma, hemangioma, pyogenic granuloma, seborrheic keratosis, basal cell carcinoma or angioma.With the help of dermoscopy, it allows doctors to better identify and diagnose the nodular melanoma according to its special dermoscopic features.
Dermoscopic features of seborrheic keratosis vs nodular melanoma
By using of dermoscopy, it allows more precise and clear visualization of skin lesions. Compared nodular melanoma with seborrheic keratosis, there are some different dermoscopic characteristics between them.
Color:
Seborrheic Keratosis (SK): There is usually white or pale yellow within the seborrheic keratosis.
Nodular Melanoma (NM): There are often 5~6 mixed colors within the lesion,blue-black color is commonly presented.
Shape:
Seborrheic Keratosis (SK):Seborrheic keratosis commonly presents like milary cyst .
Nodular Melanoma (NM): Nodular melanoma commonly presents like blood blister, crystalline.
Structure:
Seborrheic Keratosis (SK): Seborrheic Keratosis with tiny white starry or larger yellowish cloudy.
Nodular Melanoma (NM): Nodular nelanoma with disorganised asymmetrical structure, blue-grey structure, blue-black structure.
Others:
Seborrheic Keratosis (SK): There may irregular crypts,fissures/ridges, blue-grey globules, Light brown fingerprint-like parallel structures, ‘Fat fingers’ be demonstrated in the lesion.
Nodular Melanoma (NM): While, atypical vascular patterns and black-blue veil are the special features within nodular melanoma

Self-examination in nodular melanoma
Since many skin diseases resemble the nodular melanoma, it causes more difficulties to recognize nodular melanoma, especially in its early stage. Hence, it increase the importance to observe and examine by people do self-examination with dermoscopy regularly.
First of all, people should know how to use or operate dermoscopy correctly, and conditions of using dermoscopy, like related working environment. Keeping observing during the process of dermoscopy is also important. If any atypical suspicious findings which are different from normal ones, then the skin conditions should have been checked by professional dermatologists.
Importance of dermoscopy in the diagnosis of nodular melanoma
As the innovative improvement of medical instrument, dermoscopy plays a very important roles in the diagnosis of skin diseases like nodular melanoma. The whole process by dermoscopy to inspect and diagnose skin lesions is noninvasive and painless. Dermoscopy greatly reduces the cross infection during the examinations. And dermoscopy also reduces the unnecessary biopsy and surgery. Dermoscopy becomes a very popular and frequent-used device both among dermatologists and public.
Dermoscopy of Nodular Melanoma: A Clinical Guide to the Most Aggressive Skin Cancer
Nodular melanoma (NM) accounts for a disproportionate number of melanoma-related deaths due to its rapid vertical growth phase. Unlike superficial spreading melanoma, NM often fails the traditional ABCDE criteria, making nodular melanoma dermoscopy the most critical tool for early clinical intervention. This guide explores the diagnostic hallmarks of NM and the essential "EFG" rule used by dermatologists worldwide.
The Clinical Challenge: Beyond the ABCDE Rule
Nodular melanoma often presents as a symmetric, firm, and single-colored nodule, which can deceive clinicians relying on visual asymmetry alone. To improve detection, experts utilize the EFG Rule: - Elevation: The lesion is raised above the skin level. - Firmness: The nodule feels hard to the touch. - Growth: Rapid increase in size over a period of 1 to 3 months. When these clinical signs are met, an immediate dermoscopy nodular melanoma assessment is mandatory.
Key Dermoscopic Hallmarks of Nodular Melanoma
In the absence of a classic pigment network, clinicians must look for subtle micro-architectural clues that indicate high-grade malignancy.
1. Blue-White Veil
The blue-white veil is an irregular, structureless area of blue pigment with an overlying ground-glass haze. In nodular melanoma dermoscopy, this feature indicates deep dermal invasion and epidermal thickening. Achieving clarity on this veil requires superior optical systems like the IBOOLO DE-4100 Pro.
2. Polymorphous and Atypical Vascular Patterns
Since many NM lesions are hypomelanotic (lacking pigment), vascular analysis is paramount. Look for a combination of: - Atypical dotted vessels. - Linear-irregular vessels. - Milky-red globules or areas. The coexistence of these different vessel types in a chaotic arrangement is a strong predictor of nodular melanoma.
3. Crystalline Structures (Polarized Only)
Under polarized dermoscopy, "shiny white lines" or crystalline structures may become visible. These represent altered collagen bundles in the dermis and are a significant marker for invasive growth patterns that are often missed under non-polarized light.
Differential Diagnosis: Nodular Melanoma vs. Mimics
| Feature | Nodular Melanoma | Pyogenic Granuloma | Dermatofibroma |
|---|---|---|---|
| Vessels | Polymorphous (Chaotic) | Coiled/Capillary loops | Peripheral dotted |
| Structure | Blue-white veil/Atypical dots | White rail lines/Collarette | Central white patch |
| Pigment | Often absent or asymmetric | Absent | Symmetric peripheral network |
Optimizing Analysis with IBOOLO Advanced Technology
The high-stakes nature of dermoscopy for nodular melanoma requires hardware that delivers uncompromising detail. IBOOLO devices support the clinical workflow through: - High-Resolution 10x Optics: Essential for detecting the tiny atypical dots and polymorphous vessels. - Toggleable Polarization: The IBOOLO DE-3100 allows clinicians to switch instantly to polarized mode to reveal hidden crystalline structures. - Smartphone Integration: Capturing 4K images allows for immediate teledermatology consultation, which is vital when managing rapidly growing nodules.
Clinical Management and Monitoring
Due to the aggressive vertical growth of NM, the "wait and see" approach is never appropriate if suspicious dermoscopic features are present. Digital documentation via an IBOOLO smartphone adapter can help track lesion changes, but any firm, growing nodule should be prioritized for an excisional biopsy with a wide safety margin.
Frequently Asked Questions
Can nodular melanoma be skin-colored?
Yes, amelanotic variants of nodular melanoma are common. In these cases, the diagnosis relies heavily on identifying atypical vascular patterns under the dermascope.
Why is the EFG rule used for nodular melanoma?
The EFG rule (Elevation, Firmness, Growth) was developed because nodular melanoma often does not show the asymmetry or irregular borders of other melanomas in its early stages.
How does polarized light help in NM diagnosis?
Polarized light is essential for seeing "shiny white structures" and deep vascularity, which are critical clues for invasive melanoma that are often obscured by surface glare.






















