Article
Dermoscopy of Pigmented Actinic Keratosis
Pigmented Actinic Keratosis is a clinical subtype of Actinic Keratosis that manifests as hyperpigmentation and hyperkeratosis of the skin and is commonly found in areas that receive frequent sun exposure. The disease causes hyperpigmented and keratotic lesions on the skin, which severely affects the patient’s appearance and may lead to low self-esteem and social impairment….
Pigmented Actinic Keratosis is a clinical subtype of Actinic Keratosis that manifests as hyperpigmentation and hyperkeratosis of the skin and is commonly found in areas that receive frequent sun exposure. The disease causes hyperpigmented and keratotic lesions on the skin, which severely affects the patient’s appearance and may lead to low self-esteem and social impairment. Pigmented solar keratosis is a precancerous condition that, if left untreated, may develop into squamous cell carcinoma, posing a serious threat to skin health. Dermoscopy can clearly observe the characteristic manifestations of pigmented keratosis pilaris, such as hyperpigmentation, hyperkeratosis and follicular keratosis, etc., which can help doctors make a more accurate diagnosis.
Overview of Pigmented Actinic Keratosis
Pigmented actinic keratosis is primarily characterized by the occurrence of varying degrees of atypical hyperplasia of intraepidermal cells in the skin, accompanied by hyperpigmentation. It is a precancerous skin lesion. There is a strong association between pigmented solar keratosis and skin cancer. Many studies have shown that patients with actinic keratosis are more likely to develop squamous cell carcinoma.
The etiology and pathogenesis of actinic keratosis pigmentosa are not fully understood, but long-term sun exposure may be the main cause of its development. Elderly people have low DNA damage repair capacity, which predisposes them to the development of actinic keratoses. Especially white people, long-term exposure to strong ultraviolet rays as well as radiation and other ionizing radiation, more prone to disease.
Pigmented actinic keratoses tend to be limited, sharply demarcated, keratotic rashes that are flat or slightly elevated and have a normal skin color or reddish color. The surface of the skin beneath the scales is red, bumpy and papillomatous, and is easily sensitized, showing capillary dilatation and hyperpigmentation.
Pigmented Actinic Keratosis and Other Skin Lesions
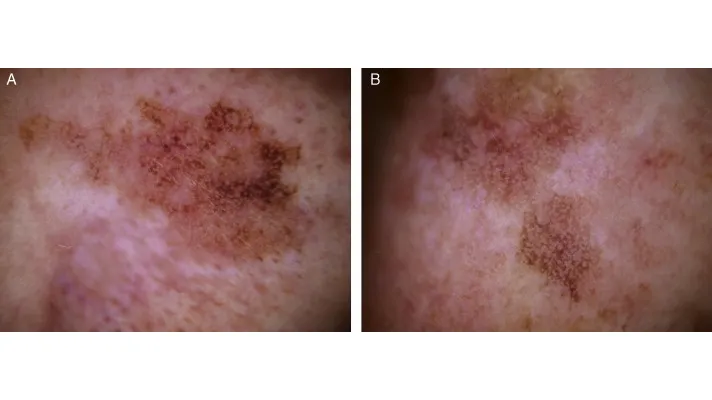
Pigmented Actinic Keratosis presents dermoscopically as erythema forming a pink-reddish vascular pseudonetwork surrounding hair follicles, yellowish-white scales, thin and wavy vessels surrounding the follicles, and follicular openings filled with keratotic plugs. These structures define the so-called “strawberry” pattern.
Pigmented solar keratoses can be clearly distinguished from other skin lesions under dermoscopy. Dermoscopic images of seborrheic keratoses usually show light or dark brown ovoid plaques with well-defined borders and a warty or keratotic surface; dermoscopic manifestations of basal cell carcinomas may include a lack of pigmented networks, large blue-grey ovoid nests with large, bluish grey globules, and multiple bluish grey spherules. These features are clearly distinguishable from the red pseudo-reticular structures and follicular keratoses of actinic keratoses.
Dermoscopy Procedure
Before performing a dermatoscopic examination, the patient needs to clean the area of skin to be examined and keep the skin dry. The probe of the dermatoscope is then applied to the surface of the skin that needs to be observed, keeping the probe at a distance from the skin and pressing it against the skin if necessary. Adjust the focus until the image is clear. DE-3100, DE-4100 and IBOOLO’s Pocket Dermatoscope series can be connected to a cell phone for image saving.
Proper skin cleansing steps and application procedures can improve the accuracy of the examination. However, the final diagnosis is still the judgment of the doctor, and an experienced doctor is the key to the correct diagnostic structure.
Dermoscopy of Pigmented Actinic Keratosis
Dermoscopy uses an optical magnification system to magnify pigmented solar keratosis lesions several times, clearly showing red grid-like structures, thread-like wavy blood vessels, and follicular openings. Dermoscopic image analysis reduces the errors of visual examination and by magnifying and clarifying the details of the skin surface, doctors are able to more accurately identify the characteristic structures of Pigmented Actinic Keratosis. Early screening and diagnosis through dermoscopy also reduces unnecessary biopsies and lowers healthcare costs.

Dermoscopy and Other Diagnostic Methods
The advantage of dermoscopy is that it magnifies the skin lesions tens to hundreds of times, which helps the doctor to observe the subtle structures and features of the skin surface more clearly, and to observe details that cannot be observed by traditional visual examination. Compared with histopathological examination, dermoscopy is a non-invasive examination and does not cause any harm to the human body. Although dermoscopy can provide detailed information on lesions, in some cases, such as lesions suspected to be malignant, further tissue biopsy is required to confirm the diagnosis.
Dermoscopy in the Management of Pigmented Actinic Keratosis
The IBOOLO dermoscopy series plays an important role in long-term patient follow-up. Regular dermoscopic examinations with IBOOLO dermatoscopes allow doctors to dynamically visualise changes in pigmented solar keratosis lesions and detect progression or recurrence of the disease in a timely manner.
By observing the pigmentation pattern of the lesion area and changes in the degree of keratinisation, doctors can determine whether treatment is effective or not and adjust the treatment plan accordingly.The IBOOLO DE-3100 and DE-4100 can be used not only for direct hand-held observation with the naked eye, but also connected to a mobile phone for image saving. The images of consecutive time periods can help doctors to evaluate the treatment effect well.

Therapeutic Strategies for Pigmented Actinic Keratosis
For dermoscopic findings that indicate mild lesions, milder treatments such as topical medications or cryotherapy may be chosen. For moderate to severe lesions, more aggressive treatments such as photodynamic therapy (PDT) or surgical excision need to be considered.
Topical medications such as fluorouracil ointment and imiquimod cream are relatively slow to work but are usually safer. When the lesions are more limited, liquid nitrogen freezing is an effective method, which is easy to operate and has a better prognosis. However, it should be noted that the freezing time should not be too long to avoid adverse reactions such as hypopigmentation.
As a non-invasive treatment method, PDT usually has a better prognosis, but adverse reactions such as erythema, edema and pain may occur during treatment. Early surgical treatment should be performed when signs of malignancy are detected or when it is not possible to determine whether the lesion is malignant. Surgical excision can completely remove the lesion and prevent further progression of the disease, although some patients may be left with scarring.
The Critical Role of Dermoscopy in the Diagnosis and Management of Pigmented Actinic Keratoses
Dermoscopy, as a non-invasive skin imaging technique, is able to eliminate reflected light from the skin surface and visualise the size and morphology of pigmented structures and superficial vascular plexus vessels within the epidermis, epidermal dermal junction, and superficial dermis, which makes dermoscopy the tool of choice for the diagnosis of pigmented skin diseases such as solar keratoses.
Continuous dermoscopy education can help the public to properly understand the importance of skin health, the dangers of skin diseases and preventive measures. This helps to reduce the incidence of skin diseases and improve people’s quality of life.
Pigmented Actinic Keratosis Dermoscopy: Key Insights - IBOOLO
IBOOLO pigmented actinic keratosis dermoscopy: Innovative detection of precancerous lesions, enabling early intervention and non-invasive skin cancer prevention.
Pigmented Actinic Keratosis Dermoscopy: A Comprehensive Guide to Early Detection and Management
Skin health is a critical aspect of overall wellness, and understanding complex dermatological conditions like pigmented actinic keratosis (PAK) can be life-saving. Pigmented actinic keratosis dermoscopy represents a cutting-edge diagnostic approach that empowers healthcare professionals to identify and manage potentially precancerous skin lesions with unprecedented precision.
Understanding the Basics of Pigmented Actinic Keratosis
Pigmented actinic keratosis is a unique dermatological condition characterized by hyperpigmented and hyperkeratotic skin lesions, primarily affecting areas exposed to prolonged sun damage. These lesions are more than just a cosmetic concern – they represent a significant risk factor for developing squamous cell carcinoma.
Risk Factors and Pathophysiology
The development of pigmented actinic keratosis is closely linked to: Prolonged sun exposure, Advanced age, Compromised DNA repair mechanisms, Fair skin complexion and Cumulative UV radiation damage.
The Revolutionary Role of Dermoscopy
Pigmented actinic keratosis dermoscopy has transformed skin lesion diagnosis by providing unprecedented visual insights. This non-invasive technique allows dermatologists to: Magnify skin structures 10-100 times, Observe subtle vascular and pigmentation patterns, Reduce unnecessary invasive procedures and Enhance early detection capabilities.
Distinctive Dermoscopic Features
Experts can identify pigmented actinic keratosis through characteristic dermoscopic signs: Erythematous vascular pseudo-network, Yellowish-white scale formations, Thin, wavy perifoollicular vessels and Keratotic follicular plugs creating a "strawberry" pattern.
Diagnostic and Treatment Strategies
Pigmented actinic keratosis dermoscopy enables precise diagnostic approaches: Diagnostic Techniques; Comprehensive skin surface examination, High-resolution imaging and Comparative analysis with standard diagnostic criteria.
Treatment Options
1. Topical Medications
2. Cryotherapy
3. Photodynamic Therapy
4. Surgical Intervention
Prevention and Long-Term Management
Effective management extends beyond treatment:
- Regular skin screenings
- Sun protection protocols
- Lifestyle modifications
- Early intervention strategies
Pigmented actinic keratosis dermoscopy represents a pivotal advancement in dermatological diagnostics. By enabling early detection and precise characterization of potentially precancerous lesions, this technique provides hope and proactive healthcare solutions.
Recommended reading
Affordable Polarized Light Dermoscopy Selection from Top China Products Supply - IBOOLO
As a leading affordable polarized light dermoscopy products supply in China, over 11+ years experience allows us to packed professional grade viewing into easy-to-carry mobile devices.
Dermoscopy Applications in the Diagnosis of Psoriasis - IBOOLO
IBOOLO Discover the powerful role of dermoscopy in diagnosing and managing psoriasis. Explore the distinctive dermoscopic features that aid in early detection and differentiation from similar skin conditions.
China's Premier Smartphone Dermoscopy Basal Cell Carcinoma Manufacturing Products Supply - IBOOLO
Through masterful production techniques, our China products supply delivers advanced yet smartphone dermoscopy basal cell carcinoma merging cutting-edge optics with compact, ergonomic frames ideal for transport and mobility.






















