Article
Dermoscopy of Scalp Psoriasis
Scalp psoriasis, a common chronic, recurrent autoimmune disease, has a definite genetic predisposition to scalp psoriasis. Its prevalence is reflected in its wide spectrum and high incidence. The scalp, due to its special physiological position, is poorly insulated and susceptible to wind-cold, thus increasing the probability of developing the disease.Dermatoscope plays an important role in…
Scalp psoriasis, a common chronic, recurrent autoimmune disease, has a definite genetic predisposition to scalp psoriasis. Its prevalence is reflected in its wide spectrum and high incidence. The scalp, due to its special physiological position, is poorly insulated and susceptible to wind-cold, thus increasing the probability of developing the disease.
Dermatoscope plays an important role in the diagnosis and treatment of scalp psoriasis. Dermoscopy is able to magnify fine skin structures. Through dermoscopy, doctors are able to observe subtle changes on the surface of the scalp, including psoriasis, intense erythematous reactions, follicular orifice plugs and burrs.
Overview of Scalp Psoriasis
Scalp psoriasis is a common chronic inflammatory skin disease characterised mainly by the appearance of reddish patches on the scalp and these patches are covered with silvery-white scales and accompanied by symptoms such as itching. It is a common type of psoriasis and one of the most common sites of lesions.
The development of scalp psoriasis is closely related to genetic factors. People with a family history of psoriasis are at a higher risk of developing it. Genetic factors may lead to abnormalities in the immune system, which in turn may trigger scalp psoriasis. Environmental factors may also play a role in the development of scalp psoriasis. For example, cold, dry climates may lead to a dry scalp, triggering or exacerbating the symptoms of scalp psoriasis.
In addition to the above pathogenesis, emotional states such as stress, anxiety, and depression may lead to an abnormal response of the immune system, which may aggravate the symptoms of scalp psoriasis.

Principles of Dermoscopy
Dermoscopy, an advanced diagnostic technique based on the principle of optical magnification and polarised light filtration, filters out the refracted light from the skin’s surface stratum corneum, allowing the observation of fine structures that are not recognisable to the naked eye. IBOOLO Dermoscopy provides a clear view of fine lesions such as erythematous spots and scales on the scalp, as well as subcutaneous haemorrhages and dilated small blood vessels.
Dermoscopy is a non-invasive, painless procedure that does not cause any harm or discomfort to the patient. This makes it the preferred screening method for patients with scalp psoriasis, especially for those who are sensitive to pain or are concerned about possible injury during the procedure.
Dermoscopic Features of Scalp Psoriasis
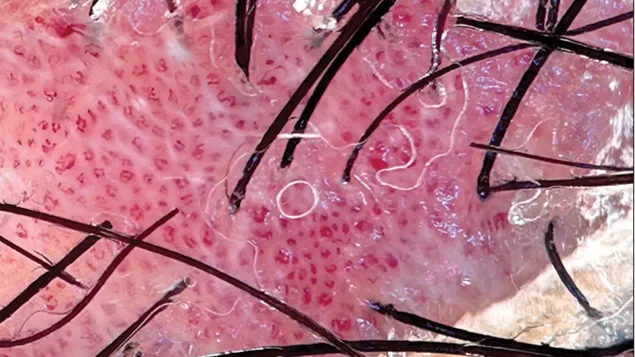
Under dermoscopy, gentle scraping of the scales from the surface of the scalp psoriasis rash reveals a pale red shiny translucent film, further scraping of this film exposes the top of the papillary layer of the dermis, where capillaries have been scraped, leading to the appearance of small haemorrhages known as punctate haemorrhages. The skin lesions of scalp psoriasis typically begin as inflammatory red papules, and the surface of the lesions is covered with multiple layers of dry, silvery-white scales, which are easily dislodged and are large in size or volume.

Dermoscopy Procedure for Patients with Scalp Psoriasis
Prior to the dermatoscopic examination, patients need to wash their hair in advance to ensure a clean scalp. The doctor will aim the probe of the dermatoscope at the scalp lesions and adjust the focal length of the dermatoscope and the intensity of the light source in order to clearly observe the fine structure and pigmentation changes on the scalp surface. The doctor will carefully observe features such as erythema, scaling, and pitting bleeding on the scalp surface and record the observations.
As a non-invasive observation tool, dermoscopy does not cause any discomfort or pain to the patient during the observation process. The entire dermoscopy process is a more relaxing experience for patients with scalp psoriasis.
How to Distinguish Scalp Psoriasis from Other Scalp Lesions
Scalp psoriasis is dermoscopically characterised by a large number of scales, which are usually flaky, thick and difficult to remove. Scalp psoriasis is often accompanied by erythema, which may be poorly defined but usually has a more pronounced inflammatory appearance.
Other scalp lesions, such as seborrheic dermatitis, are quite different dermoscopically. Seborrheic dermatitis is often accompanied by greasy and itchy symptoms, and the scales are mostly fine, greasy scales, which are different from the silver-white large scales of scalp psoriasis. The erythematous borders of seborrheic dermatitis are usually sharper and are often accompanied by perifolliculitis.

Comparison of Dermoscopy with Other Diagnostic Methods
Diagnostic accuracy: Dermoscopy and skin biopsy have relatively high diagnostic accuracy, while traditional visual examination is relatively poor.
Non-invasiveness: Dermoscopy has the advantage of being non-invasive and is suitable for use on patients of all ages, whereas skin biopsy is invasive and may cause discomfort to patients.
Cost: Conventional vision is the least expensive, dermoscopy is moderately expensive, and skin biopsy is more expensive.
Dermoscopic Images in the Management of Scalp Psoriasis
Scalp psoriasis is a chronic skin disease in which lesions change over time.IBOOLO optical dermoscopes can be connected to mobile phones for dermoscopic image storage and management, allowing doctors to compare dermoscopic images regularly to observe the development of lesions and assess the effectiveness of treatment. This dynamic monitoring helps doctors adjust the treatment plan in time to optimise the treatment effect.
Treatment Options Based on Dermoscopy
For mild to moderate scalp psoriasis, physicians may recommend topical medications such as salicylic acid, calcipotriol ointment, or tacrolimus ointment. These medications can act directly on the lesions to reduce inflammation and scaling and improve the patient’s symptoms.
Phototherapy is a physical therapy for widely distributed scalp psoriasis. It can reduce inflammation and scaling and improve skin lesions by irradiating narrow-spectrum medium-wave ultraviolet light. However, phototherapy requires long-term treatment to be effective and may bring certain side effects, such as skin sunburn and pigmentation.
Patient Education and Self-monitoring
Understanding the causes, symptoms, treatments and prognosis of scalp psoriasis will help patients reduce their fear and anxiety of the unknown, thus improving their compliance with treatment. Regular self-monitoring to observe whether the symptoms of redness, scaling and itching of the scalp are reduced or aggravated, which is helpful for the doctor to adjust the treatment plan in time.
When you want to conduct home scalp examination, then IBOOLO dermatoscope will be your best choice.IBOOLO handheld dermatoscope series can be connected to mobile phones to save dermatoscope images, easy to operate. Doctors can also use the images received to make timely judgements on the patient’s recovery and give advice.
Challenges and Future Developments in Dermoscopy
Dermoscopy of the scalp requires specialised skills. different doctors may interpret the same examination result differently, leading to inconsistent diagnosis. In the future, dermatoscopy will be combined with artificial intelligence and machine learning technologies to develop an intelligent assisted diagnosis system. The system can automatically analyse dermatoscopic images, identify lesion features and provide preliminary diagnostic recommendations.
The Critical Role of Dermoscopy in the Diagnosis and Management of Scalp Psoriasis
The ability of dermoscopy to magnify and clearly visualise fine structures and abnormal manifestations on the scalp, such as psoriasis, erythema and follicular orbital plugs, helps to accurately diagnose psoriasis and its characteristics at different stages of development.
Continuing education is vital for dermatologists, as it helps them to keep their professional knowledge up to date and keep abreast of the latest diagnostic techniques and treatments. Technological developments will make diagnosis more accurate, faster and easier, providing doctors with more comprehensive patient information and helping to develop more precise treatment plans.
Mastering Scalp Psoriasis Dermoscopy - IBOOLO
IBOOLO presents an advanced in scalp psoriasis dermoscopy, equipping clinicians with sophisticated techniques, and profound clinical insights for precise diagnosis and treatment.
Advanced Guide to Dermoscopy of Scalp Psoriasis
1. Detailed Dermoscopic Examination Process
Pre-Examination Preparation
Equipment Disinfection Standards: Before conducting dermoscopy examinations for scalp psoriasis, it is imperative to ensure that all equipment is disinfected by hospital infection control standards to prevent cross-infection. This includes wiping the equipment surface with 75% alcohol and using disposable probe covers.
Patient Skin Preparation Steps: Patients should wash their scalp before the examination to remove oils and scales, enhancing the accuracy of the examination. It is recommended to use a mild shampoo and rinse thoroughly. The examination area should be kept dry, avoiding any hair care products that might affect the results.
Environmental Lighting Requirements: The examination should be conducted under natural light or artificial light that closely resembles natural light to ensure the clarity and colour accuracy of the images. Direct light sources that may cause glare or shadows should be avoided.
Examination Techniques
Observation Methods from Different Angles: Dermoscopic examinations should be conducted from various angles to fully assess the lesions of scalp psoriasis. This includes observations perpendicular to the scalp surface and from the side to capture different light reflections.
Special Area Examination Techniques: For difficult-to-reach areas like the scalp, special probes or attachments may be required to better observe the lesion areas. Common operational mistakes include improper use of light sources, inaccurate focusing, and excessive pressure causing skin deformation, all of which can affect the results.
2. Quantitative Analysis of Dermoscopic Image Features
Erythema Intensity Grading
Erythema Intensity Grading: Erythema intensity can be divided into four levels: mild (almost invisible), moderate (visible but not affecting scalp colour), severe (obvious and darker in colour), and very severe (extremely apparent and possibly accompanied by swelling).
Measurement Methods for Extent: The extent of erythema can be measured directly or by taking photos and using software tools for measurement. Record the longest and widest diameters of erythema to assess the range of the lesion. Document the characteristics of erythema, including colour, border clarity, and desquamation or exudate.
Scale Assessment System
Scale Thickness Measurement: Using measurement tools in dermoscopy, assess the thickness of scales, categorizing them into grades from mild to severe. Distribution Pattern Classification: Categorize the patterns of scales, such as uniform distribution, patchy distribution, or clearly defined margins. Adhesion Degree Assessment: Evaluate the adhesion degree of scales, whether they are easily dislodged, and the exposure of the scalp after scale removal.
3. Dermoscopic Manifestations in Special Circumstances
Co-infections
Bacterial Infection Features: Bacterial infections may appear under dermoscopy as yellow crusts, pustules, or swollen areas. These features indicate bacterial colonization and the need for further microbiological testing and appropriate antibiotic treatment.
Fungal Infection Manifestations: Fungal infections like tinea capitis may appear under dermoscopy as grey or black dots, representing fungal spores and hyphae. Dermoscopy can also reveal inflammatory responses, such as erythema and desquamation.
Viral Infection Signs: Viral infections like herpes zoster may appear under dermoscopy as clusters of small vesicles, accompanied by significant erythema and inflammation. Dermoscopy can help differentiate viral vesicles from other types of skin lesions.
Treatment-Related Changes
Changes After Corticosteroid Treatment: After corticosteroid treatment, dermoscopy may reveal thinning of the skin, dilated capillaries, or pigmentation changes. These changes can serve as a basis for assessing treatment effectiveness and adjusting the treatment plan. Post-Phototherapy Features: Post-phototherapy, dermoscopy may show skin dryness, fine wrinkles, or pigmentation changes. These features help assess the effects of phototherapy and the skin's recovery. Responses to Biologic Treatment: Biologic treatments may lead to a reduction in skin inflammatory responses, with dermoscopy showing a decrease in erythema and scales of psoriatic lesions, indicating an improvement in condition.
4. Advanced Research Directions
Hair Follicle-Related Studies
Hair Follicle Density Measurement: Measuring hair follicle density can assess the impact of scalp psoriasis on hair growth and monitor treatment effects.
Hair Growth Cycle Assessment: Assessing the hair growth cycle can help understand the impact of scalp psoriasis on hair follicle function.
Hair Follicle Inflammation Analysis: Analyzing hair follicle inflammation can reveal the pathogenesis of scalp psoriasis and guide treatment strategies.
Vascular Pattern Research
Vascular Morphology Classification: Classifying vascular morphology, such as dilated, tortuous, or neovascularization, to understand the impact of inflammation on microcirculation.
Vascular Density Calculation: Calculating vascular density can quantify vascular changes in inflammatory areas, providing a basis for assessing disease activity.
Hemodynamic Analysis: Analyzing hemodynamics can reveal the regulatory mechanisms of vessels in response to inflammation and assess the impact of treatment on blood flow.
Recommended reading
Dermoscopy Applications in the Diagnosis of Psoriasis - IBOOLO
IBOOLO Discover the powerful role of dermoscopy in diagnosing and managing psoriasis. Explore the distinctive dermoscopic features that aid in early detection and differentiation from similar skin conditions.
basal cell carcinoma dermoscopy – IBOOLO
Shenzhen Iboolo Optics Co.Ltd has been specialized in researching and manufacturing industrial Dermatoscope, Microscope, Macro lens and Woods Lamp, since 2012. As a professional camera lens supplier, we have excellent teams who focus on products development & design, quality control & inspection and company running.
dermoscopy melanoma – IBOOLO
Shenzhen Iboolo Optics Co.Ltd established in 2012, with more than 11+ years. We have been specialized in the field of Dermatoscope, Microscope, Macro lens and Woods Lamp, and so on. We are a high-tech company integrated with research, manufacture and marketing.






















