Article
Dermoscopy of Sebaceous Hyperplasia
Sebaceous hyperplasia is commonly found on the forehead and cheeks, where lesions are localised in scattered, raised, rounded papules. Although sebaceous hyperplasia itself does not usually pose a serious health risk, it may affect the appearance to some extent, especially if the pimples appear in conspicuous places such as the face, causing psychological burden. Dermoscopy…
Sebaceous hyperplasia is commonly found on the forehead and cheeks, where lesions are localised in scattered, raised, rounded papules. Although sebaceous hyperplasia itself does not usually pose a serious health risk, it may affect the appearance to some extent, especially if the pimples appear in conspicuous places such as the face, causing psychological burden. Dermoscopy is a non-invasive test that clearly shows the features of sebaceous hyperplasia lesions, such as a yellowish background and yellowish lobulated structures. These features provide an important basis for the diagnosis of sebaceous hyperplasia.
Overview of Sebaceous Hyperplasia
Sebaceous hyperplasia is a benign lesion resulting from the enlargement of normal sebaceous glands within the skin. It is most common in people between the ages of 20 and 30, as well as in the elderly. The exact cause and pathogenesis of sebaceous hyperplasia is not fully understood. Aging of the skin, genetic factors, and endocrine disorders may all contribute to sebaceous hyperplasia. Sebaceous hyperplasia usually presents cosmetically as single or multiple, variably sized papules on the skin. These papules tend to be similar in colour to skin colour or slightly yellowish, and have a softer texture.
Skin aging is an important factor in sebaceous hypoplasia. As we age, the natural physiological processes of the skin lead to sebaceous hypoplasia, which in turn may trigger sebaceous hypoplasia. When the sebaceous glands produce too much sebum, it may lead to blockage of the follicular opening, which in turn leads to inflammation. Although sebaceous hypoplasia itself does not directly cause rosacea, both are associated with abnormal activity of the sebaceous glands.

Dermoscopy Techniques
Dermoscopy magnifies the surface of the skin through the use of an optical magnification system so that the physician can see the texture and details of the skin surface more clearly. As a result, dermoscopy can clearly show the yellow papules of sebaceous hypoplasia and the surrounding ring of blood vessels.
Before the dermoscopy begins, the area of skin to be examined needs to be thoroughly cleaned. If the IBOOLO DE-3100 is used, then next hold the lens of the DE-3100 close to the skin surface of the area to be observed and adjust the magnification and focusing distance of the dermatoscope to ensure that the details of the skin can be clearly seen during observation.
Dermoscopic Features of Sebaceous Hyperplasia
On dermoscopy, sebaceous hypoplasia usually appears as a well-defined yellow to creamy-white cloudy structure with clear borders. Telangiectasia is common but tends to be uniform.sebaceous hypoplasia usually occurs in the vicinity of hair follicles and, together with the follicles, constitutes the follicular sebaceous glandular system. Sebaceous hyperplasia can be single or multiple, and is prevalent on the forehead and cheeks, usually in a scattered distribution.
Sebaceous Hyperplasia
Basal cell carcinoma usually presents as small, pearly nodules, pink or brown in colour, with a smooth surface, sometimes accompanied by tiny vasodilatations. Sebaceous hyperplasia, on the other hand, presents mainly as an increase in the size of the sebaceous glands, with the formation of pimples, acne, greasy scales, and skin roughness. It usually appears as small nodules on the skin, ranging from a few millimetres to several centimetres in diameter, and tend to be round or oval in shape.
Dermoscopy is able to visualise structures and features of the lower epidermis, papillary dermis and deeper dermis that are not visible to the naked eye, and which have a specific and relatively clear correspondence with histopathological changes in the skin.
Dermoscopy in Therapeutic Decision-making
Sebaceous hyperplasia usually appears dermoscopically as a yellow to creamy-white cystic structure, sometimes accompanied by a central umbilical depression or opening. These features help the physician to make a definitive diagnosis of sebaceous hyperplasia so that other similar skin lesions can be ruled out. Based on dermoscopic observations, the doctor can determine the severity of sebaceous hypoplasia, the extent of the lesion and whether it is accompanied by other skin problems. For mild sebaceous hypoplasia, the doctor may recommend conservative treatments such as medication and lifestyle modifications. For moderately severe sebaceous hyperplasia or with other skin problems, doctors may recommend more aggressive treatment options such as laser therapy and surgery.
Clinical Case Study of Sebaceous Hyperplasia
Case Description:
The patient, an elderly male, presented with scattered, hemispherical, raised, yellowish papules on the forehead and cheeks. The papules were approximately 2-3 mm in diameter, soft, and commonly had an umbilical depression in the centre.
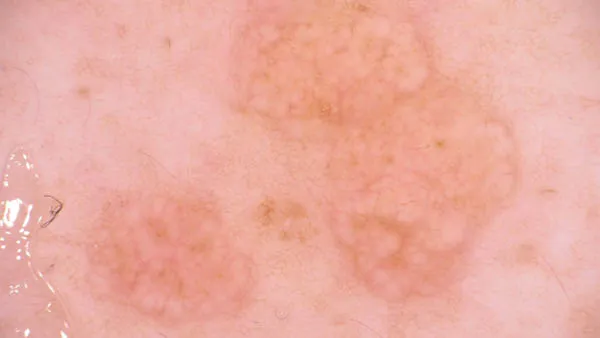
Dermoscopic images:
On dermoscopy, sebaceous hypoplasia appears as a yellowish-white nodular pattern. The openings of the glands are seen in small pits or umbilical depressions in the centre of such nodules.
Image interpretation:
The yellowish-white nodular pattern suggests hyperplasia of the sebaceous glands. The pits or umbilical recesses in the centre of the nodules are openings for sebaceous gland ducts.

Exploring Treatment Options for Sebaceous Hyperplasia
There are three main common treatment options for sebaceous hypoplasia, laser therapy, electrodesiccation and topical medication. Laser treatment involves direct application of specific wavelengths of laser light to sebaceous gland tissues. It is suitable for superficial and small amount of sebaceous hypoplasia. Electrodrying method is to use high-frequency power supply with higher voltage and lower current intensity to burn and destroy the lesion tissue. It is suitable for larger and deeper sebaceous hypoplasia. Commonly used drugs for topical medication include retinoids, antibiotics (e.g., fusidic acid cream), and anti-sebaceous hormones.
After treatment, patients should have regular rechecks so that doctors can understand the changes in the condition and adjust the treatment plan in time. If there are abnormalities, such as worsening of symptoms, relapse, etc., you should seek medical advice in time.
Strategies to Prevent Sebaceous Hyperplasia
Strategies to prevent sebaceous hypoplasia can be categorised into two main types, proper skin care and maintaining a healthy lifestyle. Skin care refers to the use of gentle cleansing products that can be used to clean the skin in daily life to avoid clogging of pores. Healthy lifestyle refers to maintaining a balanced diet, adequate sleeping time, a good state of mind, and proper physical exercise.
Daily care is essential for people with sebaceous hyperplasia who have been treated or are undergoing treatment. Skin care can help maintain clean and hygienic skin and reduce the occurrence of clogged pores and inflammation. In addition, proper diet and routine can regulate the endocrine system, thereby reducing the risk of sebaceous hypoplasia.
Sebaceous Hyperplasia Dermoscopy: Clinical Patterns & Differential Diagnosis
For dermatologists and clinicians, sebaceous hyperplasia dermoscopy is an indispensable skill. While sebaceous hyperplasia is a benign enlargement of the sebaceous glands, its clinical resemblance to Basal Cell Carcinoma (BCC) often leads to diagnostic anxiety and unnecessary biopsies. This guide provides a deep dive into the micro-architectural signatures of this condition and how to confidently differentiate it from its malignant mimics.
The Three Pillars of Sebaceous Hyperplasia Identification (H2)
Diagnosis through a dermatoscope relies on recognizing a specific "diagnostic triad." These features reflect the underlying histopathology of hypertrophied sebocytes.
1. Yellowish-White Lobular Structures (The 'Cumulus' Sign)
The hallmark of sebaceous hyperplasia is the presence of cloud-like, yellowish-white lobules. These structures represent the enlarged sebaceous gland lobules located in the upper dermis. In clinical literature, this is often referred to as the Cumulus Sign due to its resemblance to cumulus clouds.
2. Central Umbilication (The Duct Opening)
A highly specific feature is the central umbilication—a small depression or pore-like opening in the center of the lesion. Under a high-quality lens like the IBOOLO DE-4100, this appears as a whitish-yellow dot, representing the common excretory duct around which the lobules are clustered.
3. The "Crown" Vascular Pattern (Monomorphic Telangiectasia)
The vascular architecture is the most critical differentiator. Sebaceous hyperplasia typically exhibits Crown Vessels: elongated, barely branching, monomorphic telangiectasias that extend from the periphery toward the center but never cross the central umbilication. This "non-crossing" rule is vital for clinical safety.
Clinical Comparison: Sebaceous Hyperplasia vs. BCC (H2)
Misdiagnosing BCC as sebaceous hyperplasia is a high-risk clinical error. Use the following table to calibrate your observations:
| Dermoscopic Feature | Sebaceous Hyperplasia | Basal Cell Carcinoma (BCC) |
|---|---|---|
| Vessel Morphology | Crown Vessels: Peripheral, monomorphic, do not cross center. | Arborizing Vessels: Tree-like branching, sharp focus, cross the lesion center. |
| Core Structure | Central umbilication (pore-like). | Ulceration, erosion, or blue-gray nests. |
| Primary Color | Yellowish-white (opaque). | Pearly white or pinkish-red (translucent). |
| Lobulation | Present (Cloud-like appearance). | Absent (Replaced by ovoid nests/leaf-like structures). |
Advanced Techniques: Polarized vs. Non-Polarized (H2)
To maximize diagnostic accuracy, switching between lighting modes is essential:
- Polarized Light: Essential for visualizing the Crown Vessels and Rosettes without the need for immersion oil. It enhances the contrast of deeper dermal vascularity.
- Non-Polarized Light: Superior for observing the surface texture and the creamy-yellow color of the sebaceous lobules.
The IBOOLO DE-3100 allows for instantaneous toggling between these modes, ensuring no clinical detail is missed during the workflow.
Diagnostic Workflow & Patient Management (H2)
- Contextual History: Note the location (common on forehead/nose) and multiple similar lesions (suggests hyperplasia).
- Primary Sweep: Identify the yellowish "cumulus" lobules.
- Vascular Check: Confirm if vessels cross the center. If they branch sharply and cross, consider biopsy for BCC.
- Documentation: Use a smartphone adapter to capture 4K images for teledermatology consultation if the lesion is borderline.
Frequently Asked Questions (FAQ)
Can sebaceous hyperplasia be cured?
While benign and medically harmless, it can be treated for cosmetic reasons using laser therapy, cryotherapy, or electrocautery. Dermoscopy ensures the treatment is localized to the gland itself.
Why do vessels in sebaceous hyperplasia look like a 'crown'?
The "crown" appearance occurs because the vessels are pushed to the periphery by the expanding sebaceous lobules, creating a wreath-like arrangement around the central duct.
Is biopsy always necessary?
If all three dermoscopic hallmarks (yellow lobules, central pore, crown vessels) are present, the diagnostic confidence is high, and biopsies can often be avoided.
Recommended reading
basal cell carcinoma dermoscopy – IBOOLO
Shenzhen Iboolo Optics Co.Ltd has been specialized in researching and manufacturing industrial Dermatoscope, Microscope, Macro lens and Woods Lamp, since 2012. As a professional camera lens supplier, we have excellent teams who focus on products development & design, quality control & inspection and company running.
Premier China Manufacturer & Factory Supplies Affordable Polarized Dermoscopys - IBOOLO
Through streamlined China production processes, our manufacturer & factory delivers feature-rich yet affordable polarized dermoscopys designed for ergonomics, accuracy and reliable sharpness when analyzing skin.
China Skin Cancer Dermoscopy Products Supply Specializes in Professional Items - IBOOLO
Our China products supply creates clinical quality Professional skin cancer dermoscopys enabling powerful skin magnification from anywhere through thoughtful craftsmanship.






















