Article
Dermoscopy of Spitz Nevus
Spitz nevus usually occurs in children and is seen in about 15% of adolescents. Although Spitz nevus is a benign lesion, its morphology is often very similar to that of malignant melanoma, which is quite difficult to identify and easy to misdiagnose. Dermoscopy combines a microscope with polarized light that filters the refracted light from…
Spitz nevus usually occurs in children and is seen in about 15% of adolescents. Although Spitz nevus is a benign lesion, its morphology is often very similar to that of malignant melanoma, which is quite difficult to identify and easy to misdiagnose. Dermoscopy combines a microscope with polarized light that filters the refracted light from the skin’s stratum corneum to see structures that cannot be recognized by the naked eye, helping doctors better identify Spitz nevi.
Spitz Nevus Overview
Spitz nevus, also known as benign juvenile melanoma, is a benign, sporadic and well-demarcated melanotic lesion composed of bundles of ovoid or spindle-shaped epithelioid melanocytes.
Spitz nevus is often found on the face, but can also be seen on the lower limbs or trunk, and often appears suddenly and enlarges rapidly. It is more common in children and adolescents as a rare melanocytic lesion.
Spitz nevi are highly similar to malignant melanoma and both may present with spindle or epithelioid cells. Atypical Spitz nevi may have certain features of malignant melanoma, such as cellular anomalies, pathologic karyorrhexis, and a high proliferative index, which make the diagnosis more difficult.
Dermoscopy Techniques
Dermoscopy provides a clear view of the skin by filtering out diffuse reflections from the surface of the skin through a polarizing filter and selectively collecting transmitted light.Spitz nevus is a special type of pigmented nevus of the skin, whose morphology and color may vary from one individual to another. Through dermoscopy, doctors can observe the microscopic features of Spitz nevus, such as pigment distribution, vascular structure and skin texture, to assist in determining whether it is a benign lesion.
The probe of the dermatoscope is attached to the skin surface to be observed, keeping the distance between the probe and the skin, and adjusting the focus until the image is clear. Before performing dermoscopy, you should avoid applying medications or cosmetics on the skin surface to avoid physically blocking the light and affecting the imaging.
Dermoscopic Features of Spitz’s Nevus
I. Early stage of growth
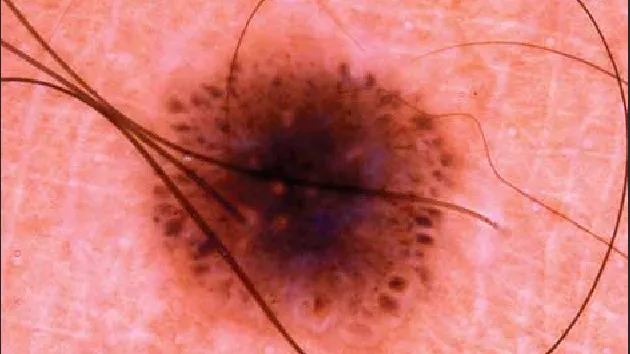
Starburst pattern is one of the typical dermoscopic manifestations of Spitz nevus, which is characterized by the presence of regularly or irregularly arranged stripes, dot balls or both around the periphery of the lesion. The spherical pattern is characterized by regular or irregular brown dot balls, which gradually become larger and merge with the growth of Spitz nevus.
II. Growth period
Streaks and punctate balls gradually increase in size and spread around the lesion. In the homogeneous pattern or the dark pigment network pattern, the pigmentation may gradually increase, making the entire lesion area more obvious and prominent.
III. Stable stage
A Spitz nevus may gradually change to a homogenous pattern, manifesting itself as diffuse uniform and structureless hyperpigmentation. In the starburst pattern, as the Spitz nevus stabilizes, the streaks and dot balls may gradually disappear or become less pronounced. This signifies that the growth of the Spitz nevus has stopped or stabilized.

Correlation of Dermoscopic Features and Histopathology of Spitz Nevus
Histopathologically the starburst pattern corresponds to the features of epidermal hyperkeratosis, thickening of the granular layer and epidermal hyperplasia; the uniformly distributed punctate vascular pattern may be related to the formation and distribution of neovascularization in Spitz nevi. In histopathology, neovascularization corresponds to areas of homogeneous dark red; a globular pattern with reticular depigmentation is associated with aggregation of melanin granules. This presentation may be associated with the proliferation and uneven distribution of melanocytes in Spitz nevi.
How to Tell the Difference Between Spitz and Melanoma
Shape: Spitz nevi are usually round or oval with clear edges; whereas melanomas are irregularly shaped with fuzzy edges.
Growth rate: A Spitz nevus grows slowly, whereas a melanoma grows faster and may increase in size rapidly over a short period of time.
Color: Spitz nevi are usually brown or black in color and are more uniform, while melanomas may vary in color and may appear blue, white, and other colors.
A Spitz nevus is a rare benign skin tumor that usually does not require treatment. However, if the mole shows abnormal changes, such as enlargement, color change, or symptoms such as pain, a medical professional will need to evaluate whether treatment is needed.

Spitz Nevus with Other Skin Lesions
Spitz nevus has clear edges, slower growth rate, uniform color and no obvious change in size. Malignant melanoma is irregularly shaped, may have bulges and ruptures on the surface, and grows faster.
Spitz nevus: dermoscopic structural patterns are mainly vascular pattern (pink homogeneous), spherical pattern, starburst pattern, reticular pattern, atypical pattern and pigmented homogeneous pattern.
Malignant melanoma: dermoscopy reveals features such as irregular vascular structures, pigmented networks, blue-white curtains, and areas of asymmetry and structurelessness.
Clinical Case Studies
Dermoscopic images clearly show microstructures and pigmentation below the skin surface, largely compensating for the limitations of clinical visualization. And there is a good correlation between most dermoscopic features and histopathologic criteria.

Guidelines for the Management of Spitz Moles
At the time of the patient’s visit, the physician should perform a detailed physical examination of the lesion, including size, shape, color, and surface features. The lesions are further examined using dermoscopy to observe the structural pattern and pigment distribution.
Spitz is a benign lesion that can be observed periodically if there are no obvious signs of discomfort; if there are changes or if the patient is concerned, laser treatment, cryotherapy or surgical excision may be considered. Patient management during treatment is equally important. Doctors should explain to patients in detail the nature of Spitz nevus, treatment options and possible risks and complications, and encourage patients to actively participate in the treatment process by asking questions and raising concerns.
Application of New Techniques in Diagnostic Dermoscopy
The use of dermoscopy in the diagnosis of Spitz nevi has provided new insights into the way nevi are observed morphologically and evolve. As technology evolves, high-resolution dermoscopy will be able to show skin structures more clearly and improve diagnostic accuracy. Combining artificial intelligence and machine learning algorithms to train models to identify and analyze specific features in dermoscopic images can assist physicians in making faster and more accurate diagnoses.
Spitz Nevus Dermoscopy: Quick Diagnosis & Monitoring Guide | IBOOLO
Learn dermoscopy for Spitz nevus, a benign lesion often confused with melanoma. Covers key features, AI tools, and telemedicine tips for better diagnosis and care.
Spitz Nevus and Dermoscopy: A Comprehensive Guide to Accurate Diagnosis and Monitoring
Spitz nevus, a benign skin lesion often seen in children and young adults, can be challenging to diagnose due to its resemblance to melanoma. Dermoscopy, a non-invasive imaging technique, has become an essential tool for dermatologists to accurately identify and differentiate Spitz nevus from more serious conditions. This blog explores the key dermoscopic features of Spitz nevus, such as the starburst pattern and homogeneous pigmentation, and provides a step-by-step guide to performing dermoscopic examinations. Additionally, it highlights the importance of quality assurance, advanced digital dermoscopy solutions, and the role of telemedicine in remote evaluation. Whether you're a healthcare professional or a patient, this guide offers valuable insights into understanding and managing Spitz nevus effectively.
What is Spitz Nevus: Understanding This Unique Skin Lesion
Spitz nevus is a type of benign skin lesion that often appears in children and young adults. It is characterized by its dome-shaped, pink or reddish appearance, and can sometimes be mistaken for melanoma due to its rapid growth and certain visual similarities. Understanding Spitz nevus is crucial for both patients and dermatologists, as it helps in making accurate diagnoses and avoiding unnecessary treatments.
- Appearance: Typically, a Spitz nevus is small, round, and symmetrical. It may have a smooth or slightly rough surface.
- Location: These lesions commonly appear on the face, neck, or legs.
- Growth: Unlike melanoma, Spitz nevus tends to grow quickly initially but then stabilizes.
Why Dermoscopy is Essential for Identifying Spitz Nevus
Dermoscopy, a non-invasive imaging technique, plays a pivotal role in the accurate identification of Spitz nevus. This method allows dermatologists to examine the skin lesion in detail, revealing patterns and structures that are not visible to the naked eye.
- Enhanced Visualization: Dermoscopy provides a magnified view of the skin, highlighting specific features such as pigment distribution and vascular patterns.
- Differentiation from Melanoma: One of the primary reasons dermoscopy is essential is its ability to help differentiate Spitz nevus from melanoma, which can have similar appearances but vastly different implications for treatment.
How to Perform Dermoscopy for Spitz Nevus: Step by Step
Performing dermoscopy on a Spitz nevus involves a systematic approach to ensure accurate analysis. Here’s a step-by-step guide:
1. Preparation: Clean the skin area and apply a gel or liquid to enhance visibility.
2. Positioning: Use a dermatoscope to position the lesion under the lens.
3. Examination: Look for key features such as:
- Starburst Pattern: A common dermoscopic feature of Spitz nevus.
- Homogeneous Pigmentation: Uniform color distribution.
- Vascular Structures: Presence of dotted or coiled vessels.
4. Documentation: Record the findings for future reference and comparison.
Can Dermoscopy Accurately Differentiate Spitz Nevus from Melanoma?
Dermoscopy is a powerful tool in distinguishing Spitz nevus from melanoma, but it requires expertise and careful analysis. While both lesions can share some visual characteristics, there are distinct dermoscopic features that can aid in differentiation.
- Starburst Pattern: More commonly seen in Spitz nevus.
- Atypical Network: Often indicative of melanoma.
- Color Variation: Melanoma typically exhibits more color variability compared to the more uniform pigmentation of Spitz nevus.
Does Dermoscopy Equipment Matter for Spitz Nevus Examination?
The quality and type of dermoscopy equipment can significantly impact the accuracy of Spitz nevus examination. Here’s a comparison of different types of dermoscopy devices:
- Traditional Dermatoscopes: Offer basic magnification and illumination but may lack advanced features.
- Digital Dermatoscopes: Provide high-resolution images and the ability to store and analyze data digitally.
- Polarized vs. Non-Polarized: Polarized dermatoscopes reduce surface reflection, offering a clearer view of deeper structures.
Key Dermoscopic Features of Spitz Nevus: A Comprehensive Guide
Understanding the key dermoscopic features of Spitz nevus is essential for accurate diagnosis. Here are some of the most important characteristics to look for:
- Starburst Pattern: Radial streaks at the periphery of the lesion.
- Globular Pattern: Round, well-defined structures within the lesion.
- Homogeneous Pigmentation: Uniform color distribution without significant variation.
- Vascular Structures: Presence of dotted or coiled vessels, often seen in Spitz nevus.
What is the Step-by-Step Workflow for Dermoscopic Examination of Spitz Nevus?
A systematic approach to dermoscopic examination ensures accurate analysis of Spitz nevus. Here’s a detailed step-by-step workflow:
1. Patient Preparation:
- Explain the procedure to the patient to ensure comfort and cooperation.
- Clean the skin area to remove any oils or debris that could interfere with imaging.
2. Equipment Setup:
- Choose a dermatoscope (polarized or non-polarized) based on the lesion’s characteristics.
- Apply a coupling agent (gel or alcohol) to enhance visibility.
3. Lesion Examination:
- Position the dermatoscope over the lesion and adjust the focus for a clear view.
- Examine the lesion systematically, starting from the periphery and moving inward.
4. Feature Identification:
- Look for key dermoscopic features such as starburst patterns, globular structures, and vascular patterns.
- Document any atypical findings that may require further investigation.
5. Image Documentation:
- Capture high-resolution images for future reference and comparison.
- Store images securely in a patient’s medical record.
6. Analysis and Diagnosis:
- Compare findings with known dermoscopic criteria for Spitz nevus.
- Consult with colleagues or use AI-based tools if uncertain about the diagnosis.
How to Perform Accurate Dermoscopy for Spitz Nevus Detection
Accurate dermoscopy for Spitz nevus detection requires a combination of technical skill, knowledge of dermoscopic features, and the right equipment. Here’s how to ensure precision:
- Understand Key Features: Familiarize yourself with the hallmark dermoscopic features of Spitz nevus, such as:
- Starburst Pattern: Radial streaks at the lesion’s edges.
- Globular Pattern: Round, well-defined structures within the lesion.
- Vascular Structures: Dotted or coiled vessels.
- Use High-Quality Equipment: Invest in a reliable dermatoscope with good magnification and illumination. Digital dermatoscopes can enhance accuracy by allowing image storage and analysis.
- Follow a Systematic Approach: Always examine the lesion in a structured manner, ensuring no areas are overlooked.
- Continuous Learning: Stay updated with the latest research and guidelines on Spitz nevus dermoscopy to refine your diagnostic skills.
Why are Clinical Applications of Dermoscopy Critical in Spitz Nevus Diagnosis?
Dermoscopy has become an indispensable tool in clinical practice for diagnosing Spitz nevus. Its applications extend beyond mere visualization, offering several critical benefits:
- Improved Diagnostic Accuracy: Dermoscopy allows dermatologists to identify subtle features that differentiate Spitz nevus from other lesions, such as melanoma.
- Non-Invasive Examination: Unlike biopsies, dermoscopy is painless and does not require tissue removal, making it ideal for pediatric patients.
- Monitoring Lesion Changes: Dermoscopy enables clinicians to track changes in Spitz nevus over time, ensuring timely intervention if needed.
- Enhanced Patient Communication: Visual aids from dermoscopy help patients understand their condition and treatment options better.
Can Dermoscopy Accurately Differentiate Spitz Nevus from Melanoma?
Dermoscopy has significantly improved the accuracy of differentiating Spitz nevus from melanoma, but it is not foolproof. Here’s what you need to know:
- Key Differentiating Features:
- Spitz Nevus: Often exhibits a starburst pattern, homogeneous pigmentation, and symmetrical structures.
- Melanoma: Typically shows irregular pigmentation, atypical networks, and asymmetrical patterns.
- Accuracy Rates: Studies suggest that dermoscopy can achieve an accuracy rate of 80-90% in distinguishing Spitz nevus from melanoma when performed by experienced dermatologists.
- Limitations: Some lesions, particularly atypical Spitz nevi, may mimic melanoma, requiring additional diagnostic methods such as biopsy or molecular testing.
What are the Latest Technological Advances in Dermoscopy for Spitz Nevus Identification?
Recent advancements in dermoscopy technology have revolutionized the identification and diagnosis of Spitz nevus. Here are some of the latest innovations:
- Digital Dermatoscopes: These devices offer high-resolution imaging and the ability to store and analyze images digitally, aiding in long-term monitoring and telemedicine consultations.
- AI-Powered Analysis: Artificial intelligence algorithms can assist dermatologists by analyzing dermoscopic images and providing diagnostic suggestions based on vast datasets.
- Polarized Light Dermatoscopy: This technology reduces surface reflection, allowing for clearer visualization of deeper structures within the lesion.
- 3D Imaging: Emerging 3D dermoscopy systems provide a more comprehensive view of the lesion’s structure, enhancing diagnostic accuracy.
- Mobile Dermatoscopy: Portable devices enable dermatologists to perform examinations in various settings, improving accessibility for patients.
What are the Specific Dermoscopic Considerations for Pediatric Spitz Nevus?
Pediatric Spitz nevus presents unique challenges and considerations in dermoscopic examination. Children often have thinner skin and more vascular lesions, which can influence the dermoscopic appearance. Here’s what to keep in mind:
- Common Features in Children:
- Starburst Pattern: Frequently observed in pediatric Spitz nevus.
- Vascular Structures: Dotted or coiled vessels are more prominent due to increased vascularity in children.
- Symmetry and Uniformity: Pediatric Spitz nevi tend to be more symmetrical and homogeneous compared to adult cases.
- Challenges:
- Lesion Growth: Rapid growth in pediatric Spitz nevus can mimic melanoma, requiring careful monitoring.
- Patient Cooperation: Younger children may be less cooperative during examination, necessitating a gentle and efficient approach.
- Best Practices:
- Use a pediatric-friendly dermatoscope with minimal contact pressure.
- Involve parents in the process to help calm and reassure the child.
Why is Quality Assurance Important in Dermoscopic Examination of Spitz Nevus?
Quality assurance in dermoscopic examination ensures consistent and accurate diagnosis of Spitz nevus, reducing the risk of misdiagnosis. Here’s why it matters:
- Consistency: Standardized protocols help maintain consistency across different examinations and practitioners.
- Accuracy: Quality assurance measures, such as regular equipment calibration and staff training, improve diagnostic accuracy.
- Patient Safety: Reducing diagnostic errors minimizes unnecessary biopsies or treatments, enhancing patient trust and outcomes.
Steps to Ensure Quality Assurance:
1. Regular Equipment Maintenance: Ensure dermatoscopes are clean, calibrated, and functioning properly.
2. Staff Training: Provide ongoing training for dermatologists and technicians on the latest dermoscopic techniques and criteria.
3. Documentation: Maintain detailed records of dermoscopic findings and follow-up actions.
4. Peer Review: Implement a system for peer review of dermoscopic images and diagnoses to identify potential errors.
How to Follow Precautions and Best Practices in Spitz Nevus Dermoscopy
Adhering to precautions and best practices is essential for accurate and safe dermoscopic examination of Spitz nevus. Here’s a step-by-step guide:
1. Patient Preparation:
- Explain the procedure to the patient to alleviate anxiety.
- Clean the skin area to remove any oils or debris.
2. Equipment Handling:
- Use a high-quality dermatoscope with appropriate magnification and lighting.
- Apply a coupling agent (gel or alcohol) to improve image clarity.
3. Examination Technique:
- Examine the lesion systematically, starting from the periphery and moving inward.
- Look for key features such as starburst patterns, globular structures, and vascular patterns.
4. Hygiene and Safety:
- Disinfect the dermatoscope before and after each use to prevent cross-contamination.
- Use disposable covers or barriers when necessary.
5. Documentation and Follow-Up:
- Capture high-resolution images for future reference.
- Schedule follow-up appointments to monitor any changes in the lesion.
What is the Maintenance and Care Guide for Dermoscopy Equipment?
Proper maintenance and care of dermoscopy equipment are crucial for ensuring accurate and reliable results. Here’s a comprehensive guide:
- Daily Care:
- Clean the lens and body of the dermatoscope with a soft, lint-free cloth.
- Use a mild disinfectant to wipe down the equipment after each use.
- Weekly Maintenance:
- Check for any signs of wear or damage, such as scratches on the lens or loose parts.
- Calibrate the dermatoscope if necessary to ensure accurate imaging.
- Storage:
- Store the dermatoscope in a protective case to prevent dust accumulation and physical damage.
- Keep the equipment in a dry, temperature-controlled environment.
- Troubleshooting:
- If the image quality deteriorates, check the lens for smudges or scratches and clean it thoroughly.
- If the device malfunctions, consult the manufacturer’s manual or contact technical support.
What are the Training Requirements for Dermoscopic Evaluation of Spitz Nevus?
Effective dermoscopic evaluation of Spitz nevus requires specialized training and continuous education. Here’s what dermatologists need to know:
- Basic Training:
- Attend accredited courses on dermoscopy to learn the fundamentals of equipment use and image interpretation.
- Study the dermoscopic features of common skin lesions, including Spitz nevus and melanoma.
- Advanced Training:
- Participate in workshops or seminars focused on challenging cases, such as atypical Spitz nevus.
- Learn to use digital dermatoscopes and AI-based diagnostic tools.
- Hands-On Experience:
- Practice dermoscopic examinations under the supervision of experienced dermatologists.
- Review and analyze a wide range of dermoscopic images to build diagnostic confidence.
- Continuous Learning:
- Stay updated with the latest research and guidelines on Spitz nevus dermoscopy.
- Engage in peer discussions and case studies to refine diagnostic skills.
When Should Primary Care Physicians Refer Patients for Spitz Nevus Evaluation?
Primary care physicians play a critical role in identifying suspicious skin lesions and determining when to refer patients to dermatologists for further evaluation of Spitz nevus. Here are the key guidelines:
- Referral Criteria:
- Rapid Growth: If the lesion shows sudden or significant growth over a short period.
- Atypical Appearance: Lesions with irregular borders, color variation, or asymmetry.
- Symptomatic Lesions: Patients reporting pain, itching, or bleeding from the lesion.
- Uncertain Diagnosis: When the primary care physician is unsure whether the lesion is a Spitz nevus or melanoma.
- Steps for Referral:
1. Document the lesion’s size, shape, color, and any changes over time.
2. Capture clinical images or use a dermatoscope if available.
3. Provide the dermatologist with a detailed patient history, including family history of skin cancer.
4. Communicate any patient concerns or symptoms clearly.
How Can Digital Dermoscopy Solutions Enhance Spitz Nevus Monitoring?
Digital dermoscopy solutions have revolutionized the monitoring of Spitz nevus by providing advanced imaging and analysis capabilities. Here’s how they can be utilized effectively:
- High-Resolution Imaging: Digital dermatoscopes capture detailed images, allowing for precise tracking of lesion changes over time.
- Image Storage and Comparison: Store dermoscopic images in a patient’s electronic health record (EHR) for easy comparison during follow-up visits.
- AI-Assisted Analysis: Some digital systems use artificial intelligence to analyze dermoscopic features, providing diagnostic suggestions and risk assessments.
- Remote Monitoring: Patients can use mobile dermatoscopy devices to capture images at home, which can be reviewed remotely by dermatologists.
Steps to Implement Digital Dermoscopy:
1. Choose a digital dermatoscope with user-friendly software and high-resolution imaging.
2. Train staff on how to operate the device and integrate it into clinical workflows.
3. Educate patients on the importance of regular monitoring and how to use mobile devices if applicable.
What are the Recommended Dermoscopic Follow-up Protocols for Spitz Nevus?
Regular follow-up is essential for monitoring Spitz nevus, especially in cases where the diagnosis is uncertain or the lesion exhibits atypical features. Here’s a step-by-step protocol:
1. Initial Examination:
- Perform a baseline dermoscopic examination and document key features.
- Capture high-resolution images for future comparison.
2. Follow-Up Schedule:
- Schedule the first follow-up visit 3-6 months after the initial examination.
- Subsequent visits can be spaced 6-12 months apart, depending on the lesion’s stability.
3. Monitoring Changes:
- Compare current dermoscopic images with baseline images to identify any changes in size, shape, or structure.
- Look for new features such as irregular pigmentation or vascular patterns.
4. Patient Communication:
- Inform patients about the importance of follow-up and encourage them to report any changes in the lesion.
How to Explain Spitz Nevus Dermoscopy Results to Patients
Effective communication of dermoscopy results is crucial for patient understanding and compliance. Here’s how to explain Spitz nevus dermoscopy results clearly and empathetically:
- Use Simple Language: Avoid medical jargon and explain terms like “starburst pattern” or “vascular structures” in plain language.
- Visual Aids: Show patients dermoscopic images to help them understand the features of their lesion.
- Discuss Implications: Explain that Spitz nevus is typically benign but requires monitoring to rule out melanoma.
- Address Concerns: Reassure patients about the low risk of malignancy and the effectiveness of regular follow-up.
Example Explanation:
“Your dermoscopy results show a lesion with a starburst pattern, which is common in Spitz nevus. This is usually a benign growth, but we’ll monitor it regularly to ensure it doesn’t change. If we notice anything unusual, we’ll take further steps.”
Can Dermoscopy Be Used for Remote Evaluation of Spitz Nevus in Telemedicine?
Dermoscopy has become a valuable tool in telemedicine, enabling remote evaluation of Spitz nevus. Here’s how it works and its benefits:
- How It Works:
- Patients or primary care providers capture dermoscopic images using mobile dermatoscopes or smartphone attachments.
- Images are securely transmitted to dermatologists for review.
- Dermatologists analyze the images and provide a diagnosis or recommend further action.
- Benefits of Remote Dermoscopy:
- Accessibility: Patients in remote or underserved areas can receive expert evaluation without traveling.
- Convenience: Reduces the need for in-person visits, saving time for both patients and providers.
- Early Detection: Enables timely identification of suspicious changes in Spitz nevus.
Steps for Implementing Remote Dermoscopy:
1. Choose a telemedicine platform that supports secure image sharing and communication.
2. Train patients or primary care providers on how to capture high-quality dermoscopic images.
3. Establish protocols for image review, diagnosis, and follow-up recommendations.
Spitz nevus is a unique skin lesion that requires careful evaluation to distinguish it from melanoma. Dermoscopy plays a critical role in this process, offering enhanced visualization and accurate differentiation through key features like the starburst pattern and vascular structures. This blog has covered essential aspects of Spitz nevus dermoscopy, including step-by-step examination protocols, the importance of quality assurance, and the latest technological advancements such as digital dermatoscopes and AI-powered analysis. Additionally, it emphasizes the significance of patient education, follow-up protocols, and the growing role of telemedicine in remote monitoring. By leveraging these tools and techniques, healthcare providers can improve diagnostic accuracy, enhance patient outcomes, and ensure effective management of Spitz nevus.
Recommended reading
China Manufacturer & Factory Specializing in Professional Dermoscopy Models - IBOOLO
Through engineering mastery nurtured over a decade, our China manufacturer & factory produces Professional dermoscopy devices combining sturdy builds and unmatched optics for flexible precision skin analysis.
dermoscopy of actinic keratosis – IBOOLO
Shenzhen Iboolo Optics Co.Ltd was established in 2012, It has been engaged in the field of Dermatoscope, Microscope, Macro lens and Woods Lamp etc. IBOOLO is a professional camera lens manufacturer with more than 11+ years experiences, which is located in Shenzhen, Guangdong.
Can dermoscopy with an electronic dermatoscope detect cancer?
Clinical studies validate that quality electronic dermatoscopes allow users to visually detect many early signs of skin cancer development with accuracy approaching in-person expert analysis. Features like asymmetry, border irregularity, evolving diameter, new colors, etc. can be recognized using an electronic dermatoscope. So combining vigilant self-checks with an electronic dermatoscope s photo documentation capabilities greatly aids early stage non-melanoma and melanoma detection.






















