Article
Skin Lesions Under IBOOLO DE-500 Dermoscope
The DE-500, launched in July 2025 as the latest model in the IBOOLO pocket dermatoscope series, represents a significant performance upgrade compared to previous devices in the same line. What’s been improved in the IBOOLO DE-500? Compared with the DE-400, the DE-500 offers three imaging modes—polarized, non-polarized, and UV—as well as three levels of brightness…
The DE-500, launched in July 2025 as the latest model in the IBOOLO pocket dermatoscope series, represents a significant performance upgrade compared to previous devices in the same line.
What’s been improved in the IBOOLO DE-500?
Compared with the DE-400, the DE-500 offers three imaging modes—polarized, non-polarized, and UV—as well as three levels of brightness adjustment. Its powerful lighting options make the DE-500 suitable for examining all types of skin lesions, and when combined with its advanced optical system, the device delivers excellent image quality.
In addition, the DE-500 uses a magnetic connection, which is more convenient than the threaded connection of the DE-400. The DE-500 also adopts an etched glass technique, whereas the DE-400 uses screen printing; etching provides clearer and more durable markings than screen printing.
What is the actual imaging performance of the IBOOLO DE-500?
Non-polarized light is mainly used to see the texture and details of the skin surface, focusing on the epidermal layer of the skin; polarized light can eliminate stray light, so that the user can clearly see the condition of the dermis layer of the skin; 365nm UV light can be used to detect fungal lesions as well as pigmentation deficiency diseases, such as vitiligo, psoriasis and so on.
The following skin lesions were all photographed with the DE-500 connected to a cell phone. According to the characteristics of different skin lesions, the user chose different lighting shots for observation.
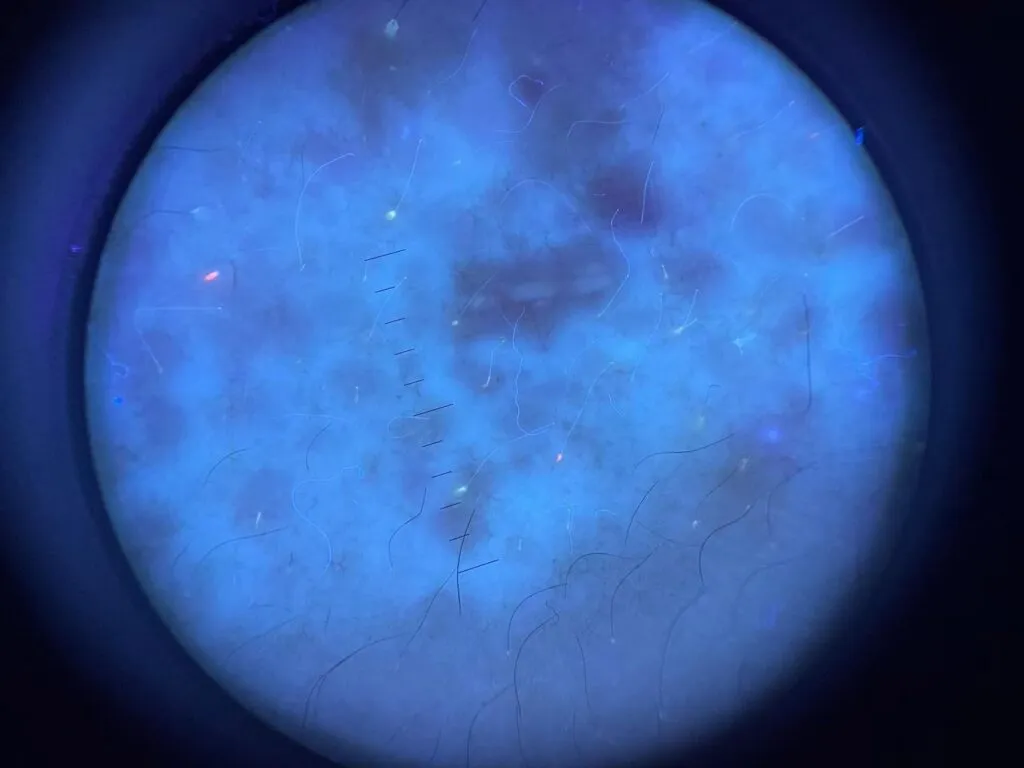
Alopecia Areata under IBOOLO DE-500
Alopecia areata under dermoscopy, also known as trichoscopy, presents several characteristic findings that are useful in clinical practice. The most consistent features include yellow dots that represent keratin and sebum in dilated follicular openings, black dots corresponding to broken hairs at the scalp surface, and exclamation-mark hairs that are tapered proximally and broader distally, often located at the border of active patches. Short vellus hairs and cadaverized hair shafts are also frequently observed, and these signs together help differentiate alopecia areata from other types of nonscarring alopecia.
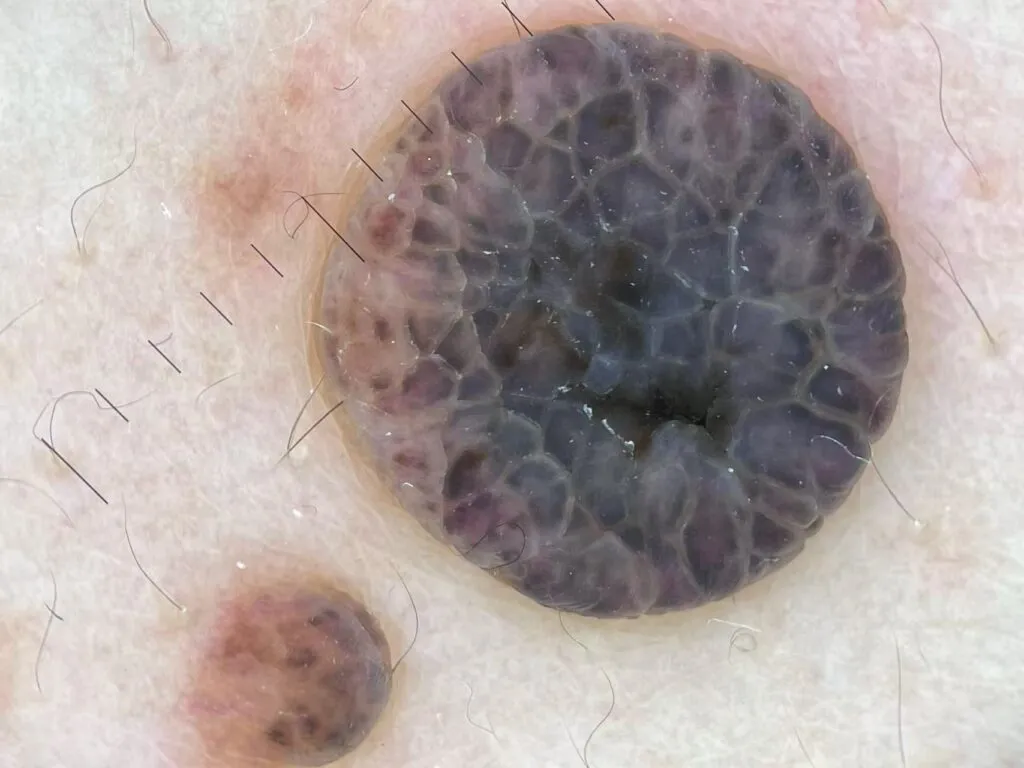
Blue Nevus under IBOOLO DE-500
Blue nevus shows on dermoscopy a homogeneous, structureless, steel-blue to blue-gray pigmentation that corresponds to melanin located in the dermis. It usually lacks a pigment network, and the blue coloration is uniform across the lesion. In some cases, blue globules or dots may be visible, and the borders tend to be well defined. These features are important for distinguishing blue nevus from malignant melanoma or other pigmented lesions.

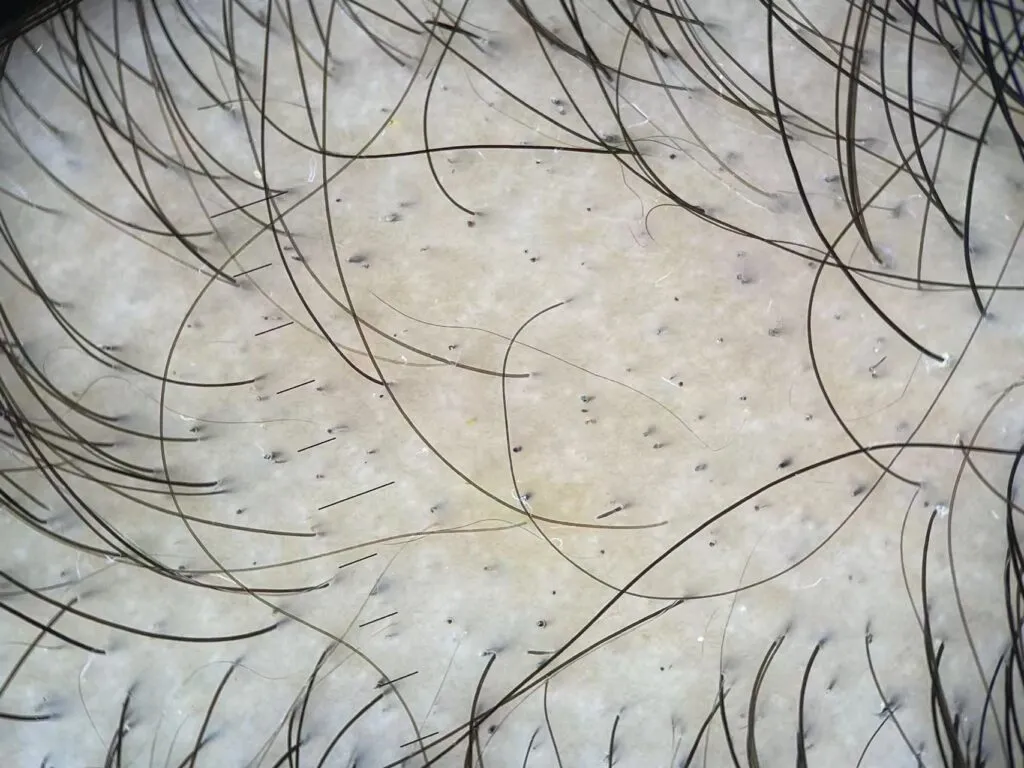
Congenital Melanocytic Nevus under IBOOLO DE-500
Congenital melanocytic nevus demonstrates variable dermoscopic patterns depending on the size and anatomic site of the lesion. Small to medium congenital nevi often show a globular or reticular-globular pattern, while larger lesions may reveal a multicomponent pattern with heterogeneous pigmentation. On the face or scalp, perifollicular pigmentation and increased follicular openings can be noted. Documenting these dermoscopic features is important to establish a baseline for long-term monitoring.

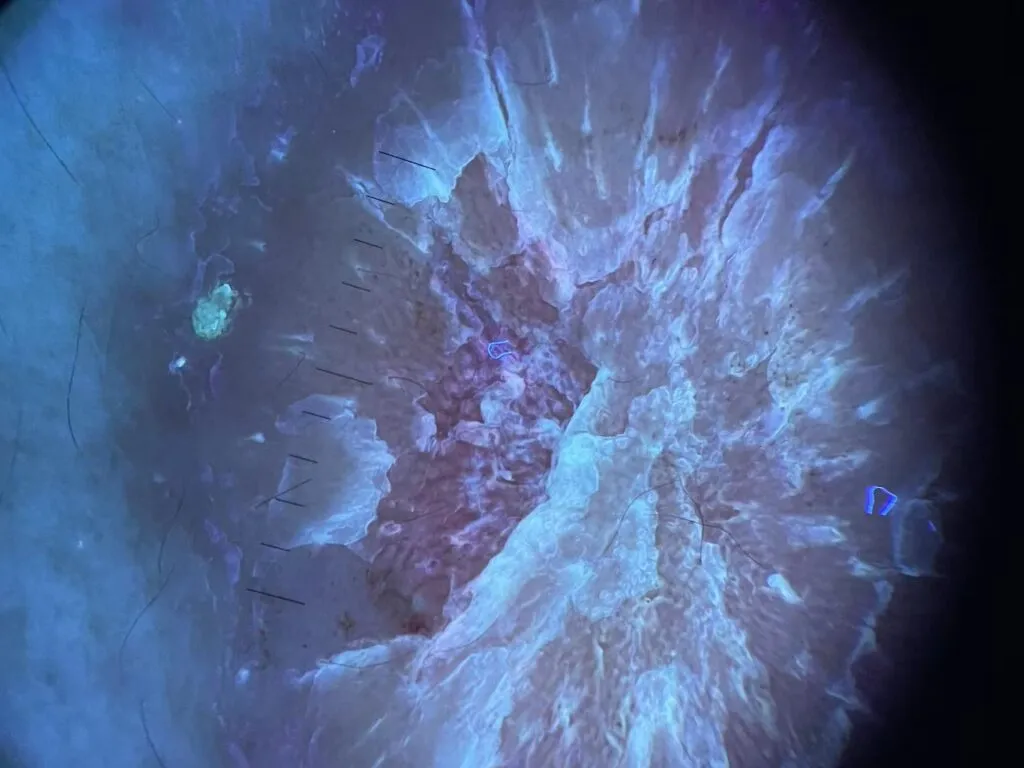
Epidermoid Cysts under IBOOLO DE-500
Epidermoid cysts under dermoscopy are characterized by the presence of a central punctum or pore, often referred to as the “pore sign.” The cyst may also show homogeneous white-yellow or yellow-brown areas reflecting keratin content. When inflamed or ruptured, vascular structures such as arborizing or branching vessels and bluish or reddish discoloration may be seen. Identifying the punctum is particularly helpful for noninvasive diagnosis.

Intradermal Nevus under IBOOLO DE-500
Intradermal nevus appears on dermoscopy as a lesion dominated by vascular rather than pigmented structures. Common findings include comma-shaped vessels and polymorphous vascular patterns on a skin-colored or slightly pigmented background. The lesion often lacks a pigment network or shows only faint pigmentation, which helps differentiate it from junctional or compound nevi and from early melanoma.
Psoriasis under IBOOLO DE-500
Psoriasis exhibits on dermoscopy a distinctive vascular and scaling pattern. The most typical features are regularly distributed red dots that correspond to dilated capillaries in dermal papillae, set against a light-red background, with overlying white scales. In plaque psoriasis, red globules and twisted red loops may also appear, arranged in a symmetrical and uniform distribution. These features aid in distinguishing psoriasis from eczema or lichen planus.
Vitiligo under IBOOLO DE-500
Vitiligo under dermoscopy is characterized by structureless white areas that lack the normal pigment network. The borders of these depigmented patches are often sharply demarcated, and perifollicular pigmentation or a reversed pigment network may be observed at the margins. Other features include leukotrichia and starburst or micro-Koebner patterns, which may indicate active disease or ongoing repigmentation. These findings support clinical diagnosis and monitoring of disease activity.