Article
What Are the Rare Skin Cancers?
Skin cancer is one of the most common types of cancer. The three most familiar types are basal cell carcinoma, squamous cell carcinoma, and malignant melanoma. However, there are also several rare skin cancers that people often overlook. This article will focus on three of them: Merkel cell carcinoma, Acral lentiginous melanoma, and Kaposi’s sarcoma.Can…
Skin cancer is one of the most common types of cancer. The three most familiar types are basal cell carcinoma, squamous cell carcinoma, and malignant melanoma. However, there are also several rare skin cancers that people often overlook. This article will focus on three of them: Merkel cell carcinoma, Acral lentiginous melanoma, and Kaposi’s sarcoma.
Can IBOOLO Dermatoscope be Used to Observe Skin Cancer?
IBOOLO offers several models, such as the DE-3100 and DE-4100, which are specifically designed for detailed skin lesion examination. These dermatoscopes utilize advanced optical technology, including polarization and non-polarization modes, to provide clear and detailed images of the skin’s surface and subsurface structures.
The IBOOLO Dermatoscope can help medical professionals and even individuals at home to monitor changes in moles, freckles, and other skin lesions, which is crucial for early detection of melanoma and other skin cancers. For example, the DE-4100 features a 10X magnification and three adjustable modes that allow users to observe skin lesions more comprehensively. Additionally, the device is portable and easy to use, making it suitable for both clinical settings and home self-examinations.

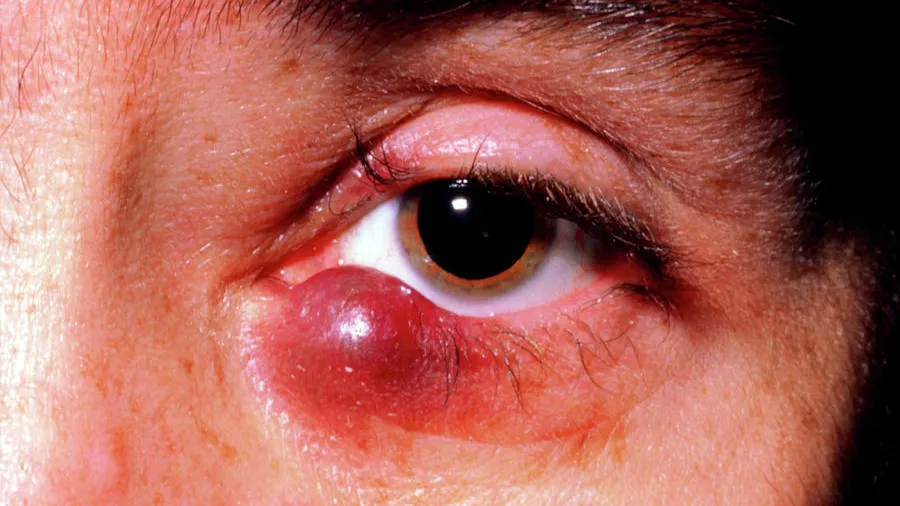
What Is Merkel Cell Carcinoma?
Merkel cell carcinoma is a rare but aggressive type of skin cancer. It usually appears on sun-exposed areas of the body, particularly the face, head, or neck. The exact cause of Merkel cell carcinoma is not fully understood. However, it’s believed to be related to a combination of factors, including UV exposure and the presence of the Merkel cell polyomavirus (MCV). Most Merkel cell tumors show evidence of this virus. Since it’s a common virus and MCC is rare, scientists are not certain about how or why the virus causes MCC in some people. What is clear is that UV exposure and immunosuppression also play a role. The tumors typically present as firm, painless lesions or nodules. They can be skin-colored, red, purple, or bluish-red. One of the distinctive features of Merkel cell carcinoma is its rapid growth, which often draws the attention of patients and doctors. Early detection is crucial as this cancer can spread quickly to other parts of the body.

What Are the Dermatoscopic Features of Merkel Cell Carcinoma?
The dermatoscopic features of Merkel cell carcinoma can vary. However, some common characteristics include a homogeneous red or pink background with irregularly distributed white areas. Telangiectasia (tiny blood vessels) may also be observed. The lesion often appears asymmetrical with irregular borders. Due to the rapid growth of Merkel cell carcinoma, these features can change quickly over time. Dermatoscopy can help in the early identification of such lesions, aiding in the prompt diagnosis and treatment of this aggressive cancer.

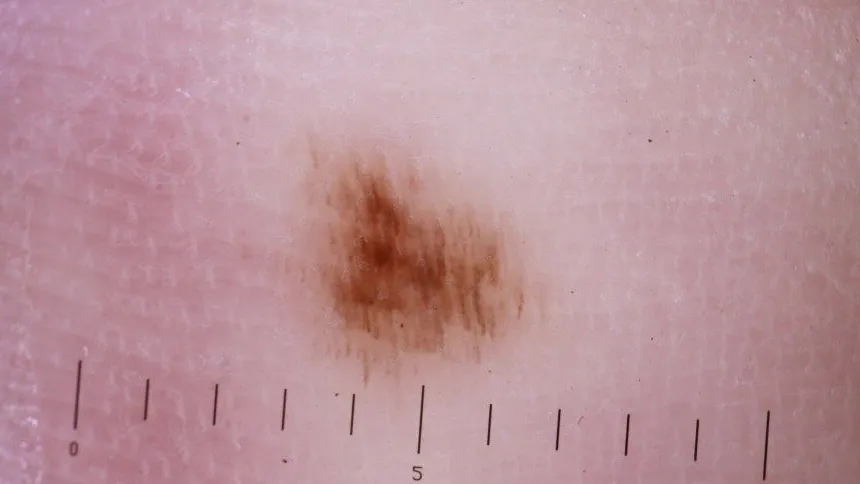
What Is Acral Lentiginous Melanoma?
Acral lentiginous melanoma is a rare and aggressive subtype of melanoma. Unlike many other types of melanoma that are linked to UV exposure, ALM is more likely caused by genetic factors. It commonly appears on hairless skin, such as the palms of the hands, soles of the feet, and under the nails. The lesions are often characterized by a black or brown color. They can be flat or slightly raised and may spread locally. ALM is the most common type of melanoma in people of color, including individuals of African ancestry. Early diagnosis is vital as this type of melanoma can be more challenging to treat once it has advanced.

What Are the Dermatoscopic Features of Acral Lentiginous Melanoma?
The dermatoscopic examination of acral lentiginous melanoma reveals several key features. These include asymmetric pigmentation with irregular brown or black streaks, especially under the nails. There may be areas of depigmentation (loss of color) within the lesion. The pigment network is often irregular, and milia-like cysts (small, white bumps) may be present. The borders of the lesion are typically irregular and blurred. These features help dermatologists differentiate ALM from other benign skin conditions that may appear similar.
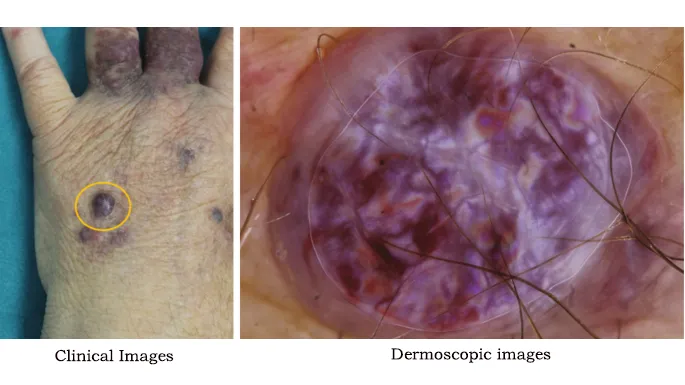
What Is Kaposi’s Sarcoma?
Kaposi’s sarcoma is a rare skin cancer that originates from the cells lining the blood vessels or lymph vessels. It is caused by the Kaposi’s sarcoma-associated herpesvirus 8 (KSHV). The disease can manifest as red, purple, or brown lesions on the skin, mucous membranes, lymph nodes, and other organs. The lesions may be flat or slightly raised and can grow and spread rapidly. Kaposi’s sarcoma is more common in individuals with weakened immune systems, such as those with HIV/AIDS, organ transplant recipients, and cancer patients receiving chemotherapy.
What Are the Dermatoscopic Features of Kaposi’s Sarcoma?
The dermatoscopic features of Kaposi’s sarcoma include purplish-red to brownish-red patches or plaques. The lesions often have a mottled appearance with areas of lighter and darker pigmentation. Telangiectasia may be visible within the lesion. The surface may appear smooth or slightly scaly. The borders can be irregular and sometimes indistinct. These characteristics help in distinguishing Kaposi’s sarcoma from other vascular lesions and skin conditions.