Article
What Causes Skin Cancer?
Skin cancer remains the most commonly diagnosed malignancy in the United States and much of the world . Although public awareness of “sun safety” has grown, incidence continues to rise for both melanoma and non-melanoma subtypes. Understanding the root causes, recognising early warning signs, and knowing when to seek professional assessment are therefore critical. What…
Skin cancer remains the most commonly diagnosed malignancy in the United States and much of the world . Although public awareness of “sun safety” has grown, incidence continues to rise for both melanoma and non-melanoma subtypes. Understanding the root causes, recognising early warning signs, and knowing when to seek professional assessment are therefore critical.
What Are the Main Drivers of Skin Cancer?
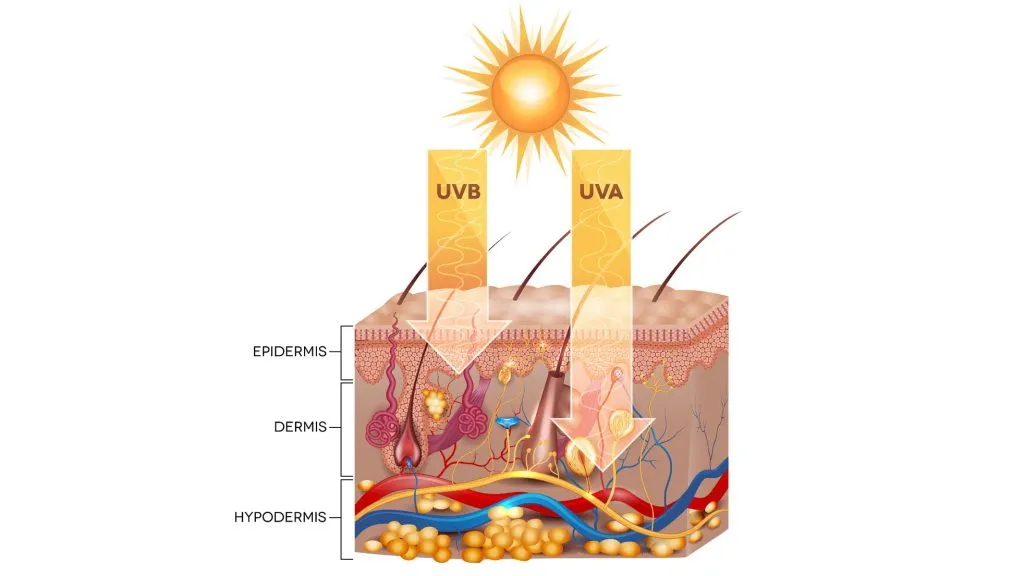
Ultraviolet (UV) radiation—both solar and artificial—stands out as the dominant external driver.
• UV-B (280–315 nm) directly induces cyclobutane pyrimidine dimers; if unrepaired, these mutations activate proto-oncogenes such as BRAF in melanocytes.
• UV-A (315–400 nm) penetrates deeper, generating reactive oxygen species that oxidise guanine bases and accelerate photo-ageing.
• Meta-analyses attribute 62–85 % of melanomas, basal-cell carcinomas (BCC) and cutaneous squamous-cell carcinomas (cSCC) to UV exposure, with intermittent blistering sunburn conferring the highest relative risk (RR 1.6–2.1) .
Artificial UV sources (tanning beds) amplify risk by 20–59 % for melanoma and 40–90 % for BCC/cSCC, especially when first exposure occurs before age 20.
Beyond light, immunosuppression (organ transplantation, biologic therapy, HIV) and inherited germline variants (CDKN2A, PTCH1) contribute.
Who Is at the Highest Risk and Why?
Genetic and phenotypic traits
• Fitzpatrick skin types I–III, red or blond hair, blue/green eyes and freckling all correlate with fewer epidermal melanin granules and therefore less natural UV shielding .
• Family history of melanoma increases lifetime risk 2- to 4-fold .
• Personal history of any skin cancer elevates the likelihood of subsequent lesions .
Environmental and lifestyle factors
• Outdoor workers accumulate chronic UV dose, leading to cSCC on the head and neck (OR 2.2) .
• Recreational sun-seekers often experience intermittent high-intensity exposure linked to superficial BCC and melanoma on the trunk .
• Alcohol intake (>15 g/day) and ionising radiation (childhood radiotherapy) further increase BCC risk (OR 1.4 and 6.3, respectively) .

How Can You Spot Skin Cancer Early?
Self-examination remains the first line of defense. The widely validated ABCDE mnemonic—Asymmetry, Border irregularity, Colour variegation, Diameter >6 mm, Evolving—detects melanomas with 92 % sensitivity when two or more criteria are present .
A – Asymmetry
Draw an imaginary line through the lesion; halves should match.
B – Border
Scalloped, notched or poorly defined edges raise suspicion.
C – Colour
Look for multiple shades of brown, black, red, white or blue within the same mole.
D – Diameter
>6 mm is the classic threshold, though early melanomas can be smaller.
E – Evolving
Any change in size, shape, colour, elevation, or new symptom (bleeding, itching) warrants prompt evaluation.

Non-melanoma clues
• BCC: pearly papule with rolled border, telangiectasia or non-healing ulcer.
• cSCC: hyperkeratotic nodule on sun-damaged skin or rapidly enlarging horn.
When Should You See a Doctor?
Immediate referral is indicated for any lesion that meets ABCDE criteria, persists beyond 4–6 weeks, ulcerates, or recurs after apparent healing . Additional red flags include:
• New pigmented lesion in an adult >40 years.
• Subungual or acral pigmentation (palms, soles) in darker skin phototypes.
• Rapid growth (>25 % in 3 months).
Can an IBOOLO dermatoscope be used to detect skin cancer?
In July 2025, IBOOLO launched its newest pocket dermatoscope—the DE-500. Compared with the DE-400, the DE-500 adds a UV light mode and three-step brightness control. Most importantly, the mounting system has been completely re-engineered. While the DE-300 and DE-400 rely on a threaded back that must be screwed into the universal phone clip, the DE-500 features a circular magnetic ring. Simply align the dermatoscope with the magnetic clip included in the kit and it snaps securely into place—faster and more convenient than ever.
Whether you are a dermatologist in clinic or a concerned patient at home, the IBOOLO DE-500 equips you with clinical-grade optics, multi-modal lighting, and instant smartphone integration to detect melanoma, basal-cell carcinoma, and squamous-cell carcinoma earlier, more accurately, and with zero invasion.

How Does a Dermatoscope Help Non-Invasively?
Traditional inspection has limitations: only 30–60 % of melanomas are correctly identified by naked-eye examination . A dermatoscope (e.g., IBOOLO’s pocket-size DE-500 or flagship DE-4100) bridges this gap by magnifying subsurface structures 10X under polarised and non-polarised light.
Key advantages
Non-invasive: No biopsies or dyes; gel coupling suffices.
Higher accuracy: Meta-analysis shows sensitivity rises to 93 % and specificity to 91 % when experienced clinicians use dermoscopy .
Instant triage: Specific patterns—reticular network, globules, blue-white veil, leaf-like areas—differentiate melanoma from benign nevus or seborrheic keratosis.
Patient empowerment: Handheld models that magnetically attach to a smartphone enable at-home documentation and tele-consultation, reducing unnecessary clinic visits.






















