Article
Dermoscopy of Actinic Keratosis
Actinic keratosis is a very common skin diseases. It is a major growing public health problem especially among older adults in white. A meta-analysis of observational studies reported by British Association of Dermatologists showed that the overall prevalence of actinic keratosis worldwide was 14%, with an estimated incidence of 1,928 cases per 100,000 people per…
Dermoscopy of Solar Actinic Keratosis Detection - IBOOLO
Explore how IBOOLO leverages dermoscopy for solar actinic keratosis diagnosis, revealing "strawberry" patterns. Learn its role in early screening, treatment monitoring, and distinguishing actinic keratosis from squamous cell carcinoma.
Dermoscopy Unveils Actinic Solar Keratosis: From Early Detection to Precision Treatment
Actinic Keratosis (AK), a common precancerous skin lesion, frequently develops on the face, hands, and other sun-exposed areas due to prolonged ultraviolet radiation exposure. If left untreated, these lesions may progress to squamous cell carcinoma. Dermoscopy of actinic keratosis has emerged as a powerful non-invasive diagnostic tool, offering high-precision visualisation that magnifies lesion details. This approach reveals characteristic features such as "strawberry-like" appearances and "fingerprint-like" structures, helping clinicians distinguish AK from squamous cell carcinoma and other skin conditions. From differentiating typical AK variants from pigmented forms and advancing toward AI-assisted diagnosis, dermoscopy not only optimises early screening but also plays a crucial role in treatment monitoring. This article explores the multidimensional applications of dermoscopy in managing actinic keratosis, providing practical insights for both patients and clinicians.
What is Actinic Keratosis?
Actinic Keratosis (AK), also known as solar keratosis, is a common skin lesion typically caused by long-term ultraviolet (UV) exposure. It presents as rough, scaly, or crusty patches on the skin, predominantly appearing on sun-exposed areas like the face, scalp, and back of hands. AK is considered a precancerous lesion—if left untreated, some cases may progress to squamous cell carcinoma (SCC). Key characteristics include:
1. Appearance: Red, brown, or skin-colored patches with rough or scaly surfaces
2. Symptoms: Possibly accompanied by itching, burning sensation, or mild pain
3. High-risk populations: Individuals with fair skin, outdoor workers, or those with a significant sun exposure history
4. Importance: Early detection and treatment of AK effectively prevent skin cancer development
What is Actinic Keratosis Under Dermoscopic Examination?
How Does Dermoscopy Reveal AK Characteristics?
In dermoscopic examination, actinic keratosis displays specific microscopic features that help clinicians accurately identify and differentiate it from other skin lesions (such as basal cell carcinoma or eczema). Dermoscopy magnifies the skin's surface and superficial structures, highlighting the unique patterns of AK. The typical manifestations include:
1. Keratotic scales: Irregular white or yellow scales on the surface, reflecting excessive keratin production
2. "Fingerprint-like" structures: Linear or reticular patterns resembling fingerprints, often appearing at lesion margins
3. Dotted or comma-shaped vessels: Irregularly distributed small vessels, indicating inflammation or neovascularisation
4. Red pseudonetwork: Background showing red reticular structures, distinct from the normal skin's pigment network
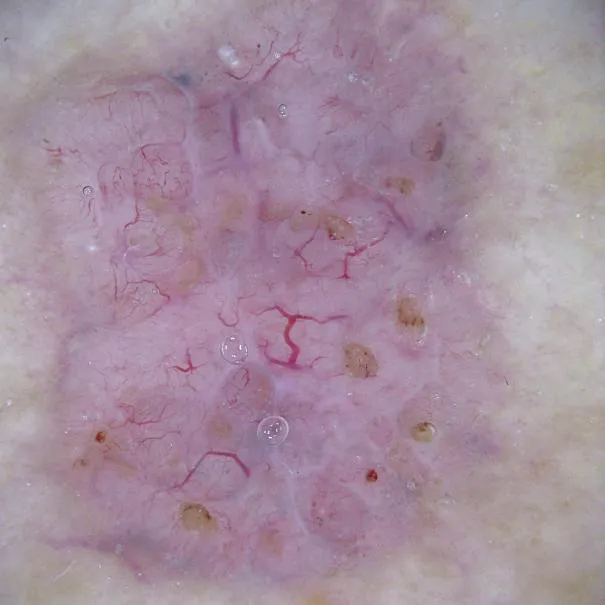
5. "Strawberry-like" appearance: Some AK lesions present with a red base accompanied by white keratotic dots, resembling strawberries
These features make dermoscopy an essential tool for AK diagnosis, particularly effective in early screening.
What Is the Step-by-Step Process for Dermoscopic Examination of Actinic Keratosis?
Dermoscopic examination is a non-invasive, painless diagnostic method used to detect actinic keratosis. The standard examination process includes:
1. Medical History Collection:
- Physician inquires about sun exposure history, when skin lesions appeared, and symptoms (such as itching or roughness)
- Gathering information about the family history of skin cancer or related risk factors
2. Visual Assessment:
- Preliminary observation of skin lesions to identify suspected AK, rough, scaly patches
- Determining areas requiring further dermoscopic examination
3. Skin Preparation:
- Cleaning the examination area to remove oils or scales, ensuring clear skin surface visibility
- If necessary, applying a liquid interface (such as gel) to enhance skin transparency
4. Dermoscopic Observation:
- Physician uses dermoscopy equipment, adjusting magnification (typically 10-50x) and light source
- Carefully examining the lesion's keratinisation patterns, vascular distribution, and background structures
5. Documentation and Diagnosis:
- Capturing lesion images for archiving and follow-up purposes
- Determining whether the lesion is AK based on dermoscopic features, or recommending biopsy to rule out malignancy
6. Follow-up Recommendations:
Physician proposes treatment plans (such as cryotherapy or topical medications) or regular monitoring schedules based on results
How Does Dermoscopy for Actinic Keratosis Work?
How Does Dermoscopy Capture AK Details?
Dermoscopic examination operates on principles of optical magnification and light optimisation technology, clearly revealing the microscopic features of actinic keratosis. Its core mechanisms include:
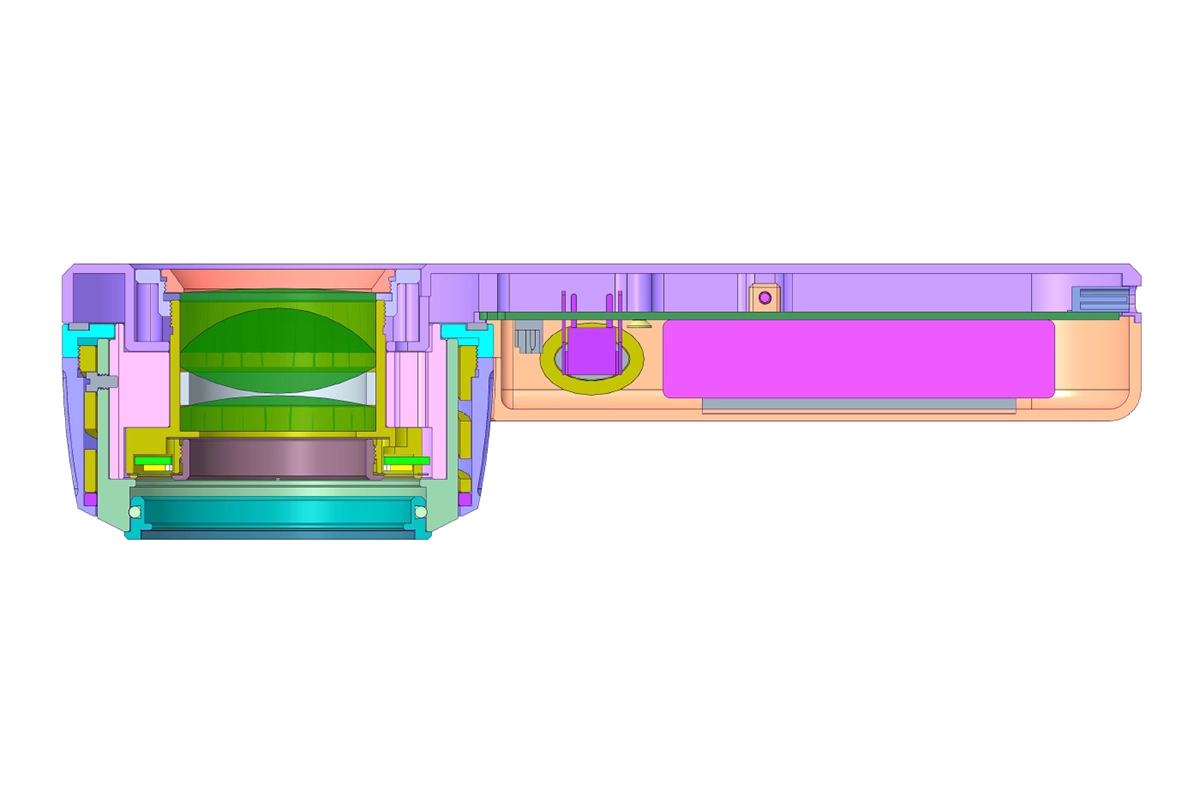
1. High-power magnification: Dermoscopy uses 10-100x magnifying lenses to reveal fine structures like keratotic scales and vascular patterns in AK
2. Light source optimisation: Devices typically feature polarised or non-polarised light. Polarised light reduces surface reflection to highlight deeper features, while non-polarised light is suitable for observing surface scales
3. Imaging and documentation: Advanced dermoscopes can connect to digital cameras or computers, recording AK lesion images for dynamic monitoring and comparison
4. Liquid interface assistance: During examination, physicians may apply alcohol or gel to the skin to improve transparency and enhance visibility of the keratin layer and blood vessels
Through these technologies, dermoscopy effectively distinguishes AK from similar lesions (such as squamous cell carcinoma or pigmented nevi), supporting precise diagnosis.
Applications of Dermoscopy in Actinic Keratosis Screening
What Roles Does Dermoscopy Play in AK Screening?
Solar keratosis dermoscopy has broad applications in screening and diagnosis, particularly suitable for high-risk populations and various clinical scenarios. Its main applications include:
1. Early screening: Identifying early-stage AK to prevent progression to squamous cell carcinoma, especially beneficial for those with long-term sun exposure or fair skin
2. Differential diagnosis: Helping distinguish AK from other skin lesions such as basal cell carcinoma, Bowen's disease, or seborrheic keratosis
3. Dynamic monitoring: Conducting regular follow-up of diagnosed AK lesions to observe change trends and evaluate treatment efficacy
4. Treatment guidance: Guiding treatment selection through assessment of AK extent and severity, such as cryotherapy, photodynamic therapy, or surgical excision
5. High-risk population management: Providing regular dermoscopic examinations for those with a family history of skin cancer or immunosuppressed patients to reduce cancer risk
6. Research and education: Dermoscopic images can be used for medical research and training, helping physicians master AK diagnostic techniques
What Are the Advantages of Dermoscopic Examination for Actinic Keratosis?
Why Choose Dermoscopy for AK Examination?
Dermoscopic examination offers significant advantages in diagnosing actinic keratosis, with its non-invasive nature and high precision making it a preferred tool in dermatology. Its main advantages include:
1. High-precision diagnosis: Dermoscopy magnifies skin details, revealing unique AK features (such as keratotic scales and "fingerprint-like" structures), improving diagnostic accuracy
2. Non-invasiveness: The examination process is painless and non-invasive, with no recovery period required, suitable for frequent screening
3. Early detection of precancerous lesions: Dermoscopy can identify early-stage AK, preventing progression to squamous cell carcinoma (SCC) and significantly reducing cancer risk
4. Reduction of unnecessary biopsies: Through preliminary screening, dermoscopy can avoid unnecessary tissue biopsies, reducing patient burden
5. Convenient follow-up: Digital image recording features support long-term monitoring of AK changes, optimising treatment management
How to Use Dermoscopy to Identify Actinic Keratosis?
Identification Process
Using dermoscopy to identify actinic keratosis requires combining equipment operation with professional knowledge. The specific operational steps are:
1. Equipment preparation:
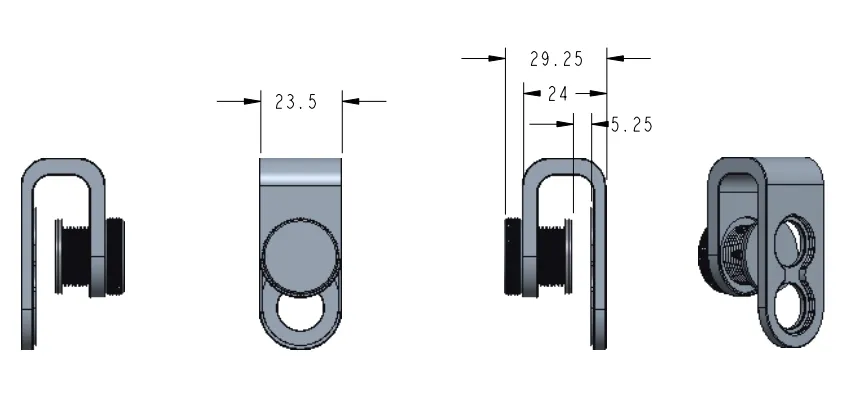
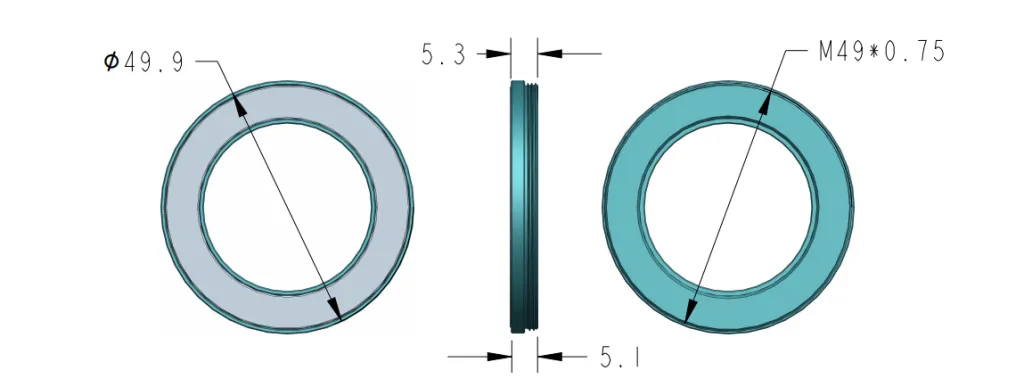
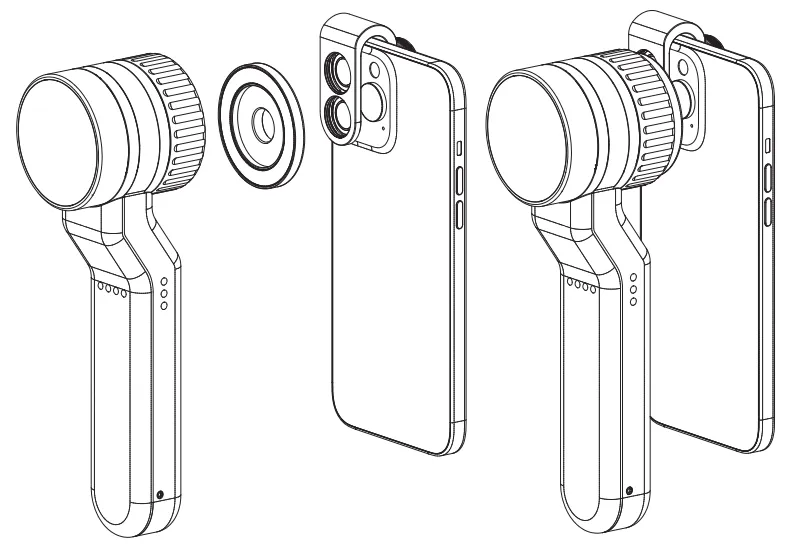
- Select high-quality dermoscopy equipment, ensuring adequate magnification (at least 10x) and light source (polarised/non-polarised) functionality
- Clean the lens and check that the light source is functioning normally
2. Skin preparation:
- Clean the patient's examination area, removing oils, scales, or cosmetics
- If needed, apply a liquid interface (such as alcohol or gel) to enhance transparency
3. Lesion observation:
- Place the dermoscope close to the target area, adjust focus and light source, and observe under magnification
- Focus on examining keratotic scales, vascular patterns (such as dotted vessels), and background structures (such as red pseudonetwork)
4. Feature documentation:
- Capture and archive lesion images, recording typical AK features like "strawberry-like" appearance or "fingerprint-like" structures
- Compare with normal skin to preliminarily determine lesion's nature
5. Consultation and verification:
- If suspicious features are found, recommend a biopsy for confirmation
- Explain observation results to patients and propose subsequent screening or treatment recommendations
Note: Non-professionals should use dermoscopy under physician guidance to avoid misdiagnosis.
What Are the Typical Dermoscopic Features of Actinic Keratosis?
What Are the Dermoscopic Characteristics of AK?
Actinic keratosis presents unique morphology and structures under dermoscopy, facilitating rapid identification. Its typical manifestations include:
1. Keratotic scales: Irregular white or yellow scales reflecting excessive keratinisation of the stratum corneum
2. "Fingerprint-like" structures: Linear or reticular patterns at margins resembling fingerprints
3. Red pseudonetwork: Red reticular structure in the lesion background, different from the normal skin's pigment network
4. Dotted or comma-shaped vessels: Small, irregularly distributed vessels indicating inflammation or vascular proliferation
5. "Strawberry-like" appearance: Red base with white keratotic dots resembling strawberries, common in inflammatory AK
6. Erosion or crusting: Some AK may present with surface damage or scabbing
These features should be analysed in combination with clinical presentation to ensure diagnostic accuracy.
What Should Be Noted During Dermoscopic Examination of Actinic Keratosis?
Key Considerations During Examination
To ensure smooth dermoscopic examination of actinic keratosis and reliable results, patients and physicians should note the following:
1. Patient preparation:
- Clean skin before examination, avoiding skincare products or cosmetics that may interfere with observation
- Inform the physician of sun exposure history, skin sensitivity history, or related symptoms (such as itching)
2. Equipment and operation:
- Use high-quality dermoscopy equipment, regularly calibrate and clean devices to ensure clear imaging
- Operation by professionally trained physicians to avoid misdiagnosis due to inexperience
3. Examination environment:
- Examine well-lit, quiet environments to reduce external interference
- Protect patient privacy, ensuring examination areas remain private
4. Result interpretation:
- Examination results should be analysed by professional dermatologists; patients should not make judgments themselves
- If suspicious features are found, promptly conduct a biopsy or further examination to rule out malignant lesions
Distinguishing Dermoscopic Features of Actinic Keratosis from Other Lesions
How to Differentiate AK from Other Lesions?
The dermoscopic features of actinic keratosis differ significantly from other skin lesions (such as basal cell carcinoma, squamous cell carcinoma, or seborrheic keratosis). Below are the main distinctions:
AK vs. Basal Cell Carcinoma (BCC):
1. AK: Primarily characterised by keratotic scales, "fingerprint-like" structures, and red pseudonetwork; vessels are mostly dotted
2. BCC: Presents "leaf-like structures," blue-grey nests, and arborising vessels, with pearl-like appearances often at margins
AK vs. Squamous Cell Carcinoma (SCC):
3. AK: Prominent keratotic features, simpler vascular patterns, more localised lesions
4. SCC: May present more significant keratotic masses, irregular vessels, and invasive margins
AK vs. Seborrheic Keratosis:
1. AK: Red base with "strawberry-like" appearance, thinner keratinisation
2. Seborrheic Keratosis: Surface presents waxy or "stuck-on" appearance, often with black or brown keratotic masses
AK vs. Pigmented Nevi:
1. AK: Lacks regular pigment network, presents an inflammatory red background
2. Pigmented Nevi: Features symmetrical pigment network and uniform pigment distribution
Through careful dermoscopic observation, physicians can effectively distinguish AK from other lesions, ensuring targeted diagnosis and timely treatment.
How to Differentiate Actinic Keratosis from Squamous Cell Carcinoma: Early Identification Points Under Dermoscopy
How Does Dermoscopy Help Distinguish AK from SCC?
As a precancerous lesion, actinic keratosis (AK) may progress to squamous cell carcinoma (SCC). Early differentiation between the two is crucial for treatment. Dermoscopy reveals unique features of both AK and SCC by magnifying lesion details. Below are key points for early identification:
AK characteristics:
- Keratotic scales: Irregular white or yellow scales reflecting excessive keratinisation
- "Fingerprint-like" structures: Linear or reticular patterns at margins
- Red pseudonetwork: Red reticular structure in the background
- Dotted/comma-shaped vessels: Small, irregularly distributed
SCC characteristics:
- Prominent keratotic masses: Thicker, uneven keratinisation layer
- Irregular vessels: Including twisted or ring-shaped vessels with more complex distribution
- Invasive margins: Blurred lesion boundaries with local destruction
- Erosion or ulceration: Common in progressive SCC
Differentiation points:
- AK lesions are typically more localised with thinner keratinisation; SCC is more invasive with significant vascular abnormalities
- If dermoscopy suggests invasive features, biopsy confirmation is needed to rule out SCC
Dermoscopic Presentation Differences Between Different Types of Actinic Keratosis (Typical, Hypertrophic, Pigmented)
What Are the Dermoscopic Features of Various AK Types?
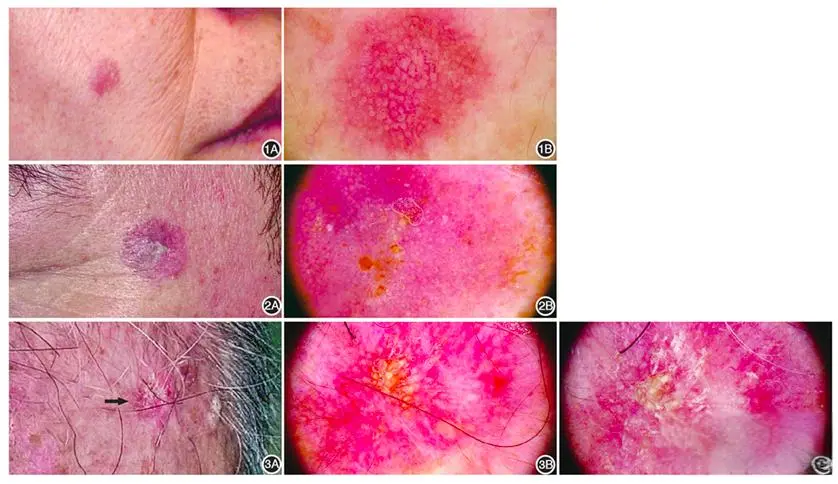
Based on clinical and histological features, actinic keratosis is classified into typical, hypertrophic, and pigmented types, each presenting differently under dermoscopy. Below are their differences:
Typical AK:
- Appearance: Red or brown patches with a rough surface and thin scales
- Dermoscopic features: Red pseudonetwork, "strawberry-like" appearance (red base with white keratotic dots), dotted vessels
- Common sites: Face, auricle, dorsum of hands
Hypertrophic AK:
- Appearance: Thicker lesions with prominent keratinisation or crusting, possibly elevated
- Dermoscopic features: Heavy white keratotic layer, irregular scale accumulation, local erosion or punctate bleeding
- Note: Requires close monitoring due to potential progression to SCC
Pigmented AK:
- Appearance: Brown or black patches, easily confused with pigmented nevi or melanoma
- Dermoscopic features: Irregular pigment network, gray-brown spots, lacking the symmetry typical of pigmented nevi
- Differentiation: Needs distinction from melanoma; may require biopsy
Understanding these differences helps physicians make precise diagnoses and develop personalised treatment plans.
Dermoscopy-Assisted Treatment Monitoring for Actinic Keratosis: Case Sharing and Analysis
How Does Dermoscopy Track AK Treatment Efficacy?
Dermoscopy is used not only for diagnosing actinic keratosis but also plays an important role in treatment monitoring. By recording changes in lesions before and after treatment, dermoscopy can evaluate efficacy and guide subsequent management. Below is an analysis of a typical case:
Case background:
- Patient: 65-year-old male with multiple facial AK, treated with cryotherapy
- Initial dermoscopic presentation: Red pseudonetwork, white keratotic scales, dotted vessels
Post-treatment monitoring:
- 1 month after: Dermoscopy showed reduced keratotic scales, faded red pseudonetwork, indicating subsiding inflammation
- 3 months after: Lesion area restored to normal skin texture, vascular patterns disappeared, indicating effective treatment
- Abnormal situations: If irregular vessels or new keratinisation remained, a biopsy would be considered to rule out SCC
Role of dermoscopy:
- Quantifying changes: Evaluating the improvement degree of keratotic layer, vessels, and background structures through image comparison
- Guiding adjustments: If efficacy is poor, may switch to photodynamic therapy or topical medications
- Preventing recurrence: Regular dermoscopic examination to monitor new lesions or recurrence
How Can Clinics Enhance Early Screening Service Quality for Actinic Keratosis Using Dermoscopy?
How to Optimise AK Screening?
The popularisation of dermoscopy technology provides clinics with opportunities to enhance early screening service quality for actinic keratosis. Below are optimisation strategies:
Equipment upgrade:
- Invest in high-quality dermoscopes (such as models supporting polarised light and digital imaging) to ensure clear images
- Regularly maintain and calibrate equipment to avoid imaging distortion
Physician training:
- Organise dermoscopy training courses focusing on AK features and differential diagnosis
- Encourage physicians to attend professional conferences like the International Dermoscopy Society to master the latest technologies
Patient education:
- Educate patients about the precancerous risks of AK, encouraging high-risk populations (such as those with long-term sun exposure) to undergo regular screening
- Use dermoscopic images to visually demonstrate lesion features, improving patient compliance
Process optimisation:
- Establish standardised screening processes, including medical history collection, dermoscopic examination, and result archiving
- Provide rapid reporting services with timely feedback on examination results
Technology integration:
- Introduce AI-assisted diagnostic tools to improve screening efficiency
- Utilise electronic medical record systems to store dermoscopic images, facilitating follow-up and multidisciplinary consultation
Through these measures, clinics can significantly improve the accuracy of AK early screening and patient satisfaction.
Dermoscopy demonstrates irreplaceable value in the diagnosis and management of actinic keratosis (AK). Through optical magnification and light optimisation technology, it precisely identifies AK features such as keratotic scales and red pseudonetwork, distinguishes between typical, hypertrophic, and pigmented AK types, and effectively differentiates from lesions like squamous cell carcinoma. The examination process is simple and non-invasive, suitable for early screening and dynamic monitoring of high-risk populations. Dermoscopy also assists in treatment efficacy evaluation, further enhancing diagnostic efficiency when combined with AI technology. Clinics can significantly optimise AK early screening services through equipment upgrades, physician training, and patient education. Whether preventing cancer progression or guiding personalised treatment, dermoscopy provides efficient and reliable solutions for AK management.
Recommended reading
Dermatoscopio Comprar: A Comparative Guide - IBOOLO
IBOOLO Comparing top dermatoscope models to help you make the best dermatoscopio comprar decision. Explore key features, capabilities, and find the device that enhances your diagnostic skills and patient care.
How can I clean my dermoscopy after usage? – IBOOLO
Cleaning your dermoscopy after usage is important to prevent cross-contamination and infection. The cleaning method may vary depending on the type and model of your dermoscopy, so you should always follow the manufacturer’s instructions. However, some general steps are: • Turn off and disconnect your dermoscopy from any power source or device. • Wipe off...
Top China Manufacturer & Factory Delivers Portable Smartphone Dermatoscopes - IBOOLO
As a premier China smartphone dermatoscope maker, our manufacturer & factory hub focuses on durability, high-fidelity optics and portable pricing to supply dermatology tools globally.
Actinic keratosis is a very common skin diseases. It is a major growing public health problem especially among older adults in white. A meta-analysis of observational studies reported by British Association of Dermatologists showed that the overall prevalence of actinic keratosis worldwide was 14%, with an estimated incidence of 1,928 cases per 100,000 people per year.
People in geographic locations with too much sun exposure are more likely to have actinic keratosis. Because there is a increasing tend that actinic keratosis translates into an risk of skin cancer, especially squamous cell carcinoma. Identifying patients at high risk for actinic keratosis and for timely and effective treatment of actinic keratosis are very important.
With the development of medical equipment, a small and flexible skin inspection tool, the dermoscope, emerged. Dermoscopy plays a crucial role in the early diagnosis, evaluation and treatment of actinic keratosis. Dermoscopy of actinic keratosis helps dermatologists make more timely and accurate analysis and judgment.Dermoscopy of actinic keratosis also enhances the confidence of doctors and patients in the treatment of actinic keratosis. Dermoscopy of actinic keratosis allows actinic keratosis to be treated more effectively.

What is Actinic Keratosis?
Actinic keratosis (shorted call AK) is also know as solar keratosis. Actinic keratoses are very common, and many people have them. It is a skin disease usually caused by long time exposure to ultraviolet light from the sun. The disease may require medical intervention, including medication or surgery, to reduce symptoms and prevent further deterioration. The best way to prevent solar keratosis is to avoid excessive exposure to the sun.
What are the Clinical Features of Actinic Keratosis?
Actinic keratosis disorders the skin to appear in thick, rough patches, itching or burning, raised wart-like growth, tenderness or pain, inflammation, increased size or thickness, multiple lesions. Actinic keratosis usually occurs in areas frequently exposed to sunlight, such as the head, arms, ears, scalp, neck, hands, face, etc.



Causes of Actinic Keratosis
It is a high risk of solar keratosis to exposure to ultraviolet (UV) radiation from the sun in long time. There are also other factors resulting in solar keratosis as below:
Long-term sunlight exposure: Long-term exposure to ultraviolet radiation from the sun is the main factor of solar keratosis.
Fair skin: People with fair skin are more susceptible to actinic keratosis. Because fair skin is more easily to receive more harmful effects of UV radiation.
Age: Actinic keratos is more commonly occurs in the middle age and old age people. Because accumulated sun exposure over time increases the posibility of developing these lesions.
History of sunburn: Severe sunburn, particularly in childhood or adolescence, increases the risk of developing actinic keratosis later in life.
Weakened immune system: Conditions or medications that weaken the immune system may also contribute to the development of solar keratosis, as the body may not be able to repair skin damage caused by UV light.
High risk Groups and Evolution
People in white, the elderly, and outdoor workers etc, are high-risk groups for actinic keratosis.
Actinic keratosis is considered a precancerous lesion because if left untreated, it can develop into skin cancer, especially squamous cell carcinoma. It is important to evaluate actinic keratosis lesions by a dermatologist and treat solar keratosis promptly to reduce the risk of skin cancer.
Dermoscopy of Actinic Keratosis
The application of dermoscopy of actinic keratosis
Dermoscopy is a non-invasive tool used to examine skin lesions. There are some main applications of dermoscopy of actinic keratosis like below:
Improved visualization: Dermatoscopy allows dermatologists to examine solar keratosis lesions more clearly, like the morphological and structural details of the lesions.
Early detection: Dermoscopy helps early detection of solar keratosis lesions for timely intervention and treatment. Early detection is essential to prevent the progressing of actinic keratoss to skin cancer.
Monitor and Evaluation: Dermoscopy can monitor the progression of solar keratosis lesions over time and evaluate of the severity of keratosis.
Differentiation from other lesions: dermoscopy can show specific features such as white scales, telangiectasia, and irregular vascular structure more clearly. It helps to distinguish solar keratosis from benign lesions such as erythema, scale, ect.

What are features of dermoscopy of actinic keratosis?
When using dermoscopy to examine actinic keratosis, several features may be observed:
Structure: Brown structure-less area, ring-shaped particle structure
Distribution: The distribution of abnormal blood vessels, such as distrubution in points, lines, etc.
Pattern: Rough and irregular surface, showing a strawberry-like pattern, a fine network of thin and dark lines
Color: Color changes such as brown or red patches, regular pigmentation, especially hyper pigmentation of hair follicle openings
Other features: redness or erythema, white or yellowish scales, small black dots similar to acne (blackheads)
Dermoscopy of actinic keratosis may vary from person to person in different populations. But the most of main or key features like above listed. Dermoscopy is much helpful to distinguish actinic keratosis from other skin diseases according to the key features of dermoscopy of actinic keratosis.
The importance of timely detection and treatment of actinic keratosis
Prompt detection and treatment of solar keratosis can help protect skin health. Early treatment can prevent worsening of the condition, prevent serious complications, and reduce the risk of skin cancer. Actinic keratosis may develop into skin cancers such as squamous cell carcinoma. However,
Dermatoscopy plays a vital role in the assessment, diagnosis and treatment of solar keratosis, helping dermatologists provide personalized and effective care for patients with this common skin disorder. Dermoscopy of actinic keratosis is closely bound up the skin examinations.
Common treatment methods of actinic keratosis
By timely detection of dermoscopy of actinic keratosis lesions, appropriate treatment measures such as cryotherapy (freezing), topical drug therapy, photodynamic therapy, chemical exfoliation or surgical removal can be taken to reduce the risk of developing skin cancer. In addition, preventive measures such as sun protection (e.g. sunscreen, wearing protective clothing, avoiding peak hours of sun) and regular skin examinations can help prevent the development of new solar keratosis lesions.
Actinic keratosis is a precancerous skin lesion. if left untreated, it can not only affect the appearance of the skin, cause pain and discomfort and also increase the risk of other skin problems. Even worse, it may develop into skin cancer, such as squamous cell carcinoma. The dermoscopy of actinic keratosis plays a very important role in the early discovery and diagnosis, as well as the detection after diagnosis, and feedback on the effects of treatment. Therefore, it is vital to develop the habit of use of dermoscopy of actinic keratosis.In addition, paying more attention to sun protection and conducting regular skin examinations are also necessary in our daily life. All these measures should be used in cooperation to reduce the potential risks faced by patients, prevent the occurrence of skin cancer, and maintain the health of the skin.