Article
Dermoscopy of Sebaceous Hyperplasia
Sebaceous hyperplasia is commonly found on the forehead and cheeks, where lesions are localised in scattered, raised, rounded papules. Although sebaceous hyperplasia itself does not usually pose a serious health risk, it may affect the appearance to some extent, especially if the pimples appear in conspicuous places such as the face, causing psychological burden. Dermoscopy…
Sebaceous hyperplasia is commonly found on the forehead and cheeks, where lesions are localised in scattered, raised, rounded papules. Although sebaceous hyperplasia itself does not usually pose a serious health risk, it may affect the appearance to some extent, especially if the pimples appear in conspicuous places such as the face, causing psychological burden. Dermoscopy is a non-invasive test that clearly shows the features of sebaceous hyperplasia lesions, such as a yellowish background and yellowish lobulated structures. These features provide an important basis for the diagnosis of sebaceous hyperplasia.
Overview of Sebaceous Hyperplasia
Sebaceous hyperplasia is a benign lesion resulting from the enlargement of normal sebaceous glands within the skin. It is most common in people between the ages of 20 and 30, as well as in the elderly. The exact cause and pathogenesis of sebaceous hyperplasia is not fully understood. Aging of the skin, genetic factors, and endocrine disorders may all contribute to sebaceous hyperplasia. Sebaceous hyperplasia usually presents cosmetically as single or multiple, variably sized papules on the skin. These papules tend to be similar in colour to skin colour or slightly yellowish, and have a softer texture.
Skin aging is an important factor in sebaceous hypoplasia. As we age, the natural physiological processes of the skin lead to sebaceous hypoplasia, which in turn may trigger sebaceous hypoplasia. When the sebaceous glands produce too much sebum, it may lead to blockage of the follicular opening, which in turn leads to inflammation. Although sebaceous hypoplasia itself does not directly cause rosacea, both are associated with abnormal activity of the sebaceous glands.

Dermoscopy Techniques
Dermoscopy magnifies the surface of the skin through the use of an optical magnification system so that the physician can see the texture and details of the skin surface more clearly. As a result, dermoscopy can clearly show the yellow papules of sebaceous hypoplasia and the surrounding ring of blood vessels.
Before the dermoscopy begins, the area of skin to be examined needs to be thoroughly cleaned. If the IBOOLO DE-3100 is used, then next hold the lens of the DE-3100 close to the skin surface of the area to be observed and adjust the magnification and focusing distance of the dermatoscope to ensure that the details of the skin can be clearly seen during observation.
Dermoscopic Features of Sebaceous Hyperplasia
On dermoscopy, sebaceous hypoplasia usually appears as a well-defined yellow to creamy-white cloudy structure with clear borders. Telangiectasia is common but tends to be uniform.sebaceous hypoplasia usually occurs in the vicinity of hair follicles and, together with the follicles, constitutes the follicular sebaceous glandular system. Sebaceous hyperplasia can be single or multiple, and is prevalent on the forehead and cheeks, usually in a scattered distribution.
Sebaceous Hyperplasia
Basal cell carcinoma usually presents as small, pearly nodules, pink or brown in colour, with a smooth surface, sometimes accompanied by tiny vasodilatations. Sebaceous hyperplasia, on the other hand, presents mainly as an increase in the size of the sebaceous glands, with the formation of pimples, acne, greasy scales, and skin roughness. It usually appears as small nodules on the skin, ranging from a few millimetres to several centimetres in diameter, and tend to be round or oval in shape.
Dermoscopy is able to visualise structures and features of the lower epidermis, papillary dermis and deeper dermis that are not visible to the naked eye, and which have a specific and relatively clear correspondence with histopathological changes in the skin.
Dermoscopy in Therapeutic Decision-making
Sebaceous hyperplasia usually appears dermoscopically as a yellow to creamy-white cystic structure, sometimes accompanied by a central umbilical depression or opening. These features help the physician to make a definitive diagnosis of sebaceous hyperplasia so that other similar skin lesions can be ruled out. Based on dermoscopic observations, the doctor can determine the severity of sebaceous hypoplasia, the extent of the lesion and whether it is accompanied by other skin problems. For mild sebaceous hypoplasia, the doctor may recommend conservative treatments such as medication and lifestyle modifications. For moderately severe sebaceous hyperplasia or with other skin problems, doctors may recommend more aggressive treatment options such as laser therapy and surgery.
Clinical Case Study of Sebaceous Hyperplasia
Case Description:
The patient, an elderly male, presented with scattered, hemispherical, raised, yellowish papules on the forehead and cheeks. The papules were approximately 2-3 mm in diameter, soft, and commonly had an umbilical depression in the centre.
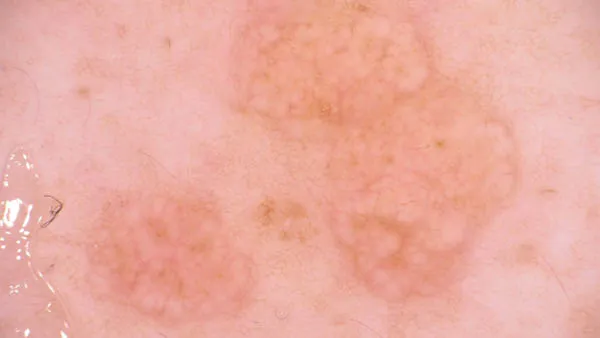
Dermoscopic images:
On dermoscopy, sebaceous hypoplasia appears as a yellowish-white nodular pattern. The openings of the glands are seen in small pits or umbilical depressions in the centre of such nodules.
Image interpretation:
The yellowish-white nodular pattern suggests hyperplasia of the sebaceous glands. The pits or umbilical recesses in the centre of the nodules are openings for sebaceous gland ducts.

Exploring Treatment Options for Sebaceous Hyperplasia
There are three main common treatment options for sebaceous hypoplasia, laser therapy, electrodesiccation and topical medication. Laser treatment involves direct application of specific wavelengths of laser light to sebaceous gland tissues. It is suitable for superficial and small amount of sebaceous hypoplasia. Electrodrying method is to use high-frequency power supply with higher voltage and lower current intensity to burn and destroy the lesion tissue. It is suitable for larger and deeper sebaceous hypoplasia. Commonly used drugs for topical medication include retinoids, antibiotics (e.g., fusidic acid cream), and anti-sebaceous hormones.
After treatment, patients should have regular rechecks so that doctors can understand the changes in the condition and adjust the treatment plan in time. If there are abnormalities, such as worsening of symptoms, relapse, etc., you should seek medical advice in time.
Strategies to Prevent Sebaceous Hyperplasia
Strategies to prevent sebaceous hypoplasia can be categorised into two main types, proper skin care and maintaining a healthy lifestyle. Skin care refers to the use of gentle cleansing products that can be used to clean the skin in daily life to avoid clogging of pores. Healthy lifestyle refers to maintaining a balanced diet, adequate sleeping time, a good state of mind, and proper physical exercise.
Daily care is essential for people with sebaceous hyperplasia who have been treated or are undergoing treatment. Skin care can help maintain clean and hygienic skin and reduce the occurrence of clogged pores and inflammation. In addition, proper diet and routine can regulate the endocrine system, thereby reducing the risk of sebaceous hypoplasia.
Sebaceous Hyperplasia Dermoscopy: Skin Lesion Insights - IBOOLO
Sebaceous Hyperplasia Dermoscopy by IBOOLO reveals precise skin imaging. Non-invasive techniques detect subtle changes, offering accurate diagnosis of this common condition.Sebaceous Hyperplasia Dermoscopy: A Comprehensive Diagnostic and Management Guide
Distinguishing from Similar Conditions
Accurately differentiating sebaceous hyperplasia from other skin lesions is crucial for appropriate management. The complexity of sebaceous hyperplasia dermoscopy lies in the subtle yet significant morphological and dermoscopic variations:
Basal Cell Carcinoma (BCC)
Visual Distinctions: BCC: Pearly, translucent appearance with irregular borders. Sebaceous Hyperplasia: Uniform, yellow-white, well-defined structures revealing characteristic sebaceous hyperplasia dermoscopy features.
Dermoscopic Indicators: BCC: Arborizing blood vessels, blue-gray ovoid nests. Sebaceous Hyperplasia: Consistent vascular pattern, central umbilication distinctive in sebaceous hyperplasia dermoscopy analysis.
Skin Tags (Acrochordons)
Structural Differences: Skin Tags: Pedunculated, soft, skin-colored growths. Sebaceous Hyperplasia: Sessile, slightly raised, yellow-white papules with unique dermoscopic characteristics.
Key Diagnostic Markers: Skin Tags: Irregular surface, variable size. Sebaceous Hyperplasia: Uniform size, consistent color pattern evident in detailed sebaceous hyperplasia dermoscopy examination.
Comparative Characteristics
Milia: Tiny, white, keratin-filled cysts. Sebaceous Hyperplasia: Larger, yellow-tinted, glandular structures with distinctive dermoscopic features.
Dermoscopic Evaluation and
Milia: Bright white, crystalline appearance. Sebaceous Hyperplasia: Soft, translucent yellow background typical of sebaceous hyperplasia dermoscopy findings.
Treatment Approaches: Personalized Intervention Strategies
Conservative Management
Conservative treatments represent the first-line approach for managing sebaceous hyperplasia, focusing on minimal intervention and symptom management:
Topical Treatments
1. Retinoid-Based Therapies
- Mechanism: Regulate sebaceous gland activity
- Examples: Tretinoin, adapalene
- Benefits: Reduce glandular hyperplasia, Improve skin texture and Minimal side effects.
2. Chemical Exfoliants
Active Ingredients: Salicylic acid, Glycolic acid and Lactic acid.
Therapeutic Goals: Normalize skin cell turnover, Reduce sebum production and Improve overall skin appearance.
Treatment Selection Criteria
Determining the most appropriate intervention requires a comprehensive assessment:
Comprehensive Evaluation Parameters
1. Clinical Considerations:
Lesion size and quantity, Location on the body, Patient's aesthetic concerns and Potential psychological impact.
2. Patient-Specific Factors
Age and skin type:Medical history, Previous treatment responses and Potential contraindications.
3. Risk-Benefit Analysis
Invasiveness of procedure, Potential scarring, Recovery time and Long-term efficacy.
Lifestyle and Preventive Strategies
Comprehensive Lifestyle Recommendations
1. Nutritional Interventions
Anti-inflammatory diet, Omega-3 fatty acid supplementation, Reduced sugar intake and Increased hydration.
2. Stress Management
Mindfulness practices, Regular exercise, Adequate sleep and Stress reduction techniques.
3. Environmental Protection
Daily broad-spectrum sunscreen, Protective clothing, Avoiding excessive sun exposure and Pollution mitigation strategies.
Proactive Skin Management
A holistic approach to skin health extends beyond individual treatments:
Integrated Skin Care Approach
1. Professional Monitoring
Regular dermatological check-ups, Advanced imaging technologies and Comprehensive skin assessments.
2. Personalized Skincare Regimens
Tailored cleansing routines, Specialized moisturization and Targeted treatment protocols.
3. Early Intervention Strategies
Continuous skin evaluation, Prompt addressing of changes and Preventive maintenance.
Patient Communication: Empowerment Through Understanding
1. Educational Approach
- Demystifying the condition
- Explaining medical terminology
- Providing comprehensive information
2. Emotional Support
- Addressing cosmetic concerns
- Managing psychological impacts
- Building patient confidence
3. Treatment Expectation Management
- Realistic outcome discussions
- Potential treatment limitations
- Long-term management strategies
Recommended reading
Dermoscopy of Dermatofibroma – IBOOLO
A dermatofibroma is a common benign bump in the skin.Dermatofibroma is usually harmless and typically appears on the lower legs. Dermatofibroma is easily mistaken from other skin tumors due to its appearance. This brings much difficult to diagnose. Hence, how to exactly diagnose dermatofibroma is special important to dermatology filed. What is dermatofibroma...
dermoscopy melanoma – IBOOLO
Shenzhen Iboolo Optics Co.Ltd established in 2012, with more than 11+ years. We have been specialized in the field of Dermatoscope, Microscope, Macro lens and Woods Lamp, and so on. We are a high-tech company integrated with research, manufacture and marketing.
Affordable digital dermatoscopes dermoscopy price - IBOOLO
IBOOLO-wide selection affordable of digital dermatoscopes for skin exams and lesion analysis offers competitively priced dermatoscopes with advanced imaging and measurements for precise dermoscopy.






















