Article
Dermoscopy of Superficial Basal Cell Carcinoma
Basal cell carcinoma is the most common skin cancer. Basal cell carcinoma rates have jumped sharply in the last years, particularly North America, Europe and selected parts of Asia. As BCC is slow-growing, then the majority are curable and cause little harm if diagnosed early and treated. Accompanied by the advances in medical technology, dermoscopy…
Clinical Guide: Mastering Superficial BCC Dermoscopy for Early Diagnosis
In modern dermatological practice, the clinical identification of superficial basal cell carcinoma (sBCC) remains a frequent challenge. Often presenting as localized, erythematous, and scaly plaques, sBCC is easily misdiagnosed as eczema or psoriasis. However, the integration of superficial bcc dermoscopy has fundamentally changed the diagnostic landscape, allowing clinicians to distinguish malignant architecture from benign inflammation with high precision.
At IBOOLO, we specialize in high-resolution optical solutions that empower clinicians to visualize the minute vascular and structural changes essential for sBCC detection. This guide provides a deep dive into the hallmark patterns, technological requirements, and differential diagnosis of superficial basal cell carcinoma.
Hallmark Patterns in Superficial BCC Dermoscopy
While all basal cell carcinomas share certain features, the dermoscopic profile of the superficial subtype is distinct. Unlike the thick, prominent vessels of nodular BCC, superficial bcc dermoscopy reveals more subtle, yet highly specific indicators.
1. Short Fine Telangiectasias (SFT)
One of the most predictive features in superficial bcc dermoscopy is the presence of short fine telangiectasias. These are delicate, minimally branching vessels that are much shorter and less pronounced than the classic "arborizing" vessels found in deeper BCC variants. Identifying these subtle vascular signatures is often the first step in differentiating sBCC from chronic dermatitis.
2. Leaf-like and Maple Leaf-like Areas
Commonly found at the periphery of the lesion, maple leaf-like areas are well-demarcated, pigmented structures that do not originate from a pigment network. These brown, gray, or blue-black patterns are direct representations of the multi-focal nest growth characteristic of superficial basal cell carcinoma.
3. Shiny White-Red Structureless Areas
Under polarized dermoscopy, sBCC often exhibits a characteristic pink-white or red-white structureless background. This is frequently accompanied by multiple small erosions or "micro-ulcerations," which appear as red-to-brownish crusts. This combination of features is a powerful indicator of malignancy in scaly, red skin patches.
Differential Diagnosis: Distinguishing sBCC from Mimics
The primary clinical utility of superficial bcc dermoscopy is its power of differentiation. By identifying specific vascular and structural motifs, clinicians can avoid unnecessary steroid treatments for misdiagnosed inflammatory conditions.
| Feature | Superficial BCC (sBCC) | Psoriasis / Eczema |
|---|---|---|
| Vascular Pattern | Short Fine Telangiectasias / Arborizing | Regular Red Dotted Vessels |
| Scale Features | Focal, yellowish or translucent | Diffuse, silvery-white or greasy |
| Pigmentation | Maple leaf-like / Blue-gray ovoid nests | Typically absent |
Optimizing Clinical Workflow with IBOOLO Optics
The success of superficial bcc dermoscopy is highly dependent on light control. Polarized light is particularly essential for visualizing "shiny white streaks" and subsurface vascularity without the need for interface fluids. IBOOLO professional dermatoscopes, such as the DE-4100 Pro, provide the 4K clarity required to resolve the extremely fine SFT vessels that characterize early sBCC.
By utilizing digital documentation and smartphone integration, clinicians can perform longitudinal monitoring. This is especially useful for sBCC, as these lesions are slow-growing. Tracking changes in vascular density or the emergence of micro-erosions over several months can provide definitive evidence for biopsy decisions, ensuring that no potential malignancy is overlooked.
Mastering the nuances of superficial bcc dermoscopy is an invaluable skill that transforms clinical outcomes. From recognizing the subtle "short fine telangiectasias" to identifying peripheral "maple leaf-like areas," the right technology and training allow for early, life-saving detection.
Recommended reading
Dermatoscope of Basal Cell Carcinoma – IBOOLO
Dermatoscope of Basal Cell Carcinoma Basal cell carcinoma (BCC) is the most common skin cancer in humans. In all over the world, the incidence of basal cell carcinoma accounts for at least 80% of skin cancers besides melanoma and 32% of all cancers. BCC mainly occurs in Caucasians and is very rare in people with...
Dermoscopy of skin cancers like basal cell carcinoma - IBOOLO
dermoscopy Skin cancer improves clinical recognition of malignancies like melanoma and basal cell carcinoma. IBOOLO innovative dermatoscopes visualize indicators unnoticeable to the unaided eye.
Download DOC Report – IBOOLO
IBOOLO is a optical lens manufacturer based in China with more than 11+ years of experience in manufacturing, catering to a variety of requirements. We have become experts in the design and manufacture of a wide variety of Dermatoscope, Woods Lamp, Microscope and Macro lens.
Basal cell carcinoma is the most common skin cancer. Basal cell carcinoma rates have jumped sharply in the last years, particularly North America, Europe and selected parts of Asia. As BCC is slow-growing, then the majority are curable and cause little harm if diagnosed early and treated. Accompanied by the advances in medical technology, dermoscopy as a non-invasive optical diagnostic tool is playing an ever-growing role for detecting superficial basal cell carcinoma at early stage.
What is superficial basal cell carcinoma?
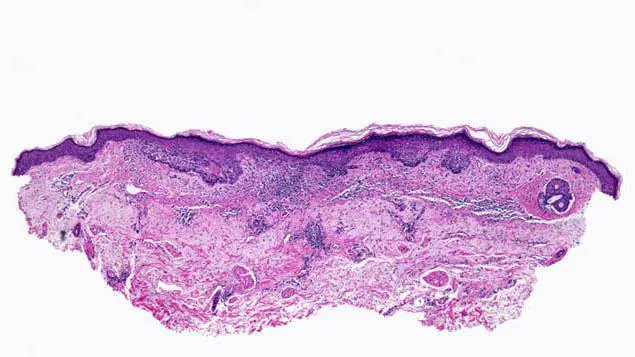
Basal cell carcinoma often referred to as basaloid is the most common type of skin cancer. It starts as a basaloid low-grade malignancy of the basal layer of epidermis or outer root sheath of hair follicles. Morphologically from clinical standpoint basal cell carcinoma can be mostly classified as: nodular-ulcerative type, superficial type, pigmented like. Basal cell carcinoma has multifactorial causes, but many cases have demonstrated a clear association with chronic sun exposure and ionizing radiation. Superficial basal cell carcinoma, a subtype of BCC that presents as red, scaly plaques on the skin, often resembling eczema or psoriasis.
Basal cell carcinoma can present in diverse clinical manifestations. The texture of these lesions tends to be firm, the surface is smooth or slightly elevated as well with a noticeable pigmentation. Basal cell carcinomas are most common on the head and neck, where they almost always affect sun-exposed areas; such as around your nose, eyelids or cheeks.

Dermoscopic features of basal cell carcinoma
Dermoscopy is useful in detecting the specific features of BCC. Some common dermoscopic characteristics are as follows:
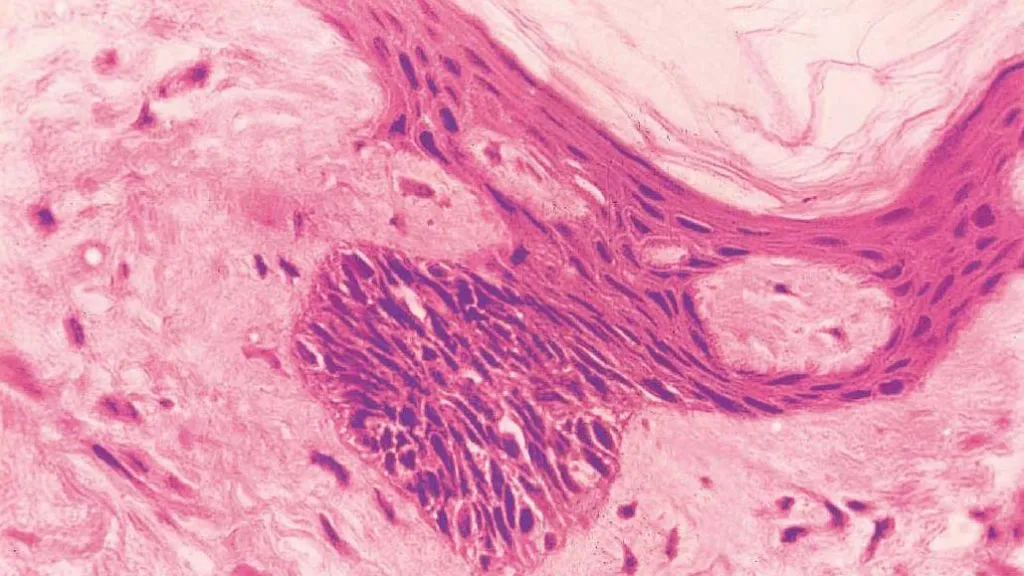
Dendritic blood vessels: Most classic dermoscopic presentations of BCC include dendritic blood vessels, which are often found in the superficial and nodular types on this lesion.
Blue-gray globules: These blobs are round or oval structures, varying in size but relatively homogeneous, and blue-gray in color on dermoscopic examination. They indicate the presence of melanin within the tumor and are commonly seen in hyperpigmented basal cell carcinoma.
Ulcers: Ulcers represent breaks or flat depres- sions in the skin, and they are observed on dermoscopy as areas of structurelessness that can appear red to orange.
Crusting: A crust is a hard cover that forms on the surface of ulcers. A crust, a yellowish or brown spot at the center of the lesion.
Superficial basal cell carcinoma features
Clinicopathological study to differentiate if a basal cell carcinoma is superficial, the morphology and growth pattern of each lesion should be evaluated. Superficial basal cell carcinomas often present as a single or multiple mildly infiltrating, erythematous scaly plaque that grows slowly and largely limits itself to the epidermis.
The often seen superficial basal cell carcinoma on the trunk, especially the back. The superficial form appears as a flat, thin red or pink patch while the sclerosing shape is characterized by thick patches that are flesh-colored or light rose and resemble scars to some extent.

Differential diagnosis of basal cell carcinoma
By dermoscopy basal cell carcinoma commonly demonstrates a pink-to-red structureless area with or without central ulceration/armor. They are more common in older individuals and usually appear on parts of the body that get lots of sun. Clinically, basal cell carcinoma is a multifaceted and multiform disease that can make subtyping challenging.
Dermoscopically melanomas have an irregular structure and shape in a multitude of colors particularly reds, blues and blacks. Although most melanomas are larger than 6 mm in diameter, early lesions can mimic benign pigmented nevi but not be noticed by the naked eye.
Dermoscopically squamous cell carcinoma has a squamous surface with visible keratin. Squamous cell infiltrative growth can be misleading to benign skin lesions such as keratosis pilaris.
Dermoscopic features and diagnostic difficulties in atypical basal cell carcinoma
Sclerosing basal cell carcinoma:
Features: white, without structure, with small twining serpentine blood vessels and many brown spots.
Challenge: Scar-like frequently and hard to differentiate from a benign scar or other sclerotic disorders.
Superficial basal cell carcinoma:
Features: fine translucent rolled margin, scattering of microerosions and mild scaling.
Challenge: Similar to inflammatory skin conditions such as eczema or psoriasis.
Cystic Basal Cell Carcinoma:
Features: soft jelly-like contents with a translucent appearance.
Challenge: confused with benign cystic lesions.
Clinical applications of dermoscopic images
Dermatoscopic images can aid in accurate sampling of biopsies when they need to be done and also decrease the unnecessary number. Characteristics of skin lesions in dermoscopy images enable experienced doctors to provide diagnoses of the type of skin cancer, and plan appropriate treatments for patients with a high speed. Furthermore, dermoscopy as a hand-held and non-invasive instrument can be easily used by the doctors to exam patients during their subsequent visits without serious of invasions that offers no discomforts for the patient; thus it may help improving compliance from patients.
The important role of dermoscopy in the treatment of basal cell carcinoma
Treatment options depend on the site and stage of the cancer, and surgery with or without adjuvant radiotherapy plays a major role in resectable basal cell carcinoma. The mainstay of treatment for limited basal cell carcinoma is surgery, and radiotherapy may be used in adjacent and complex areas, but metastatic patients will not have any hope other than benefit from systemic drug therapy.
The significance of dermoscopy in the early detection of superficial basal cell carcinoma
Many moles are invisible and some changes can only be visualized by dermoscopy, so patients should undergo routine comprehensive skin evaluation, especially of sun-exposed skin surfaces. Dermoscopy has new implications in the prevention and early diagnosis of superficial basal cell carcinoma. Dermoscopy allows visualization of the surface of skin lesions and subepidermal structures that are not visible to the naked eye through optical magnification, immersion or polarized lenses. Skin lesions revealed by dermoscopy results can be detected and managed as potentially cancerous skin lesions prior to higher cancer risk or under/over-treatment.
Patient education and self-examination
If you have a wound on your skin that has not healed after a few weeks, or if you experience redness, swelling, please seek medical attention promptly. This can be an early sign of skin cancer. In your daily life, pay attention to whether there are any new moles growing on your skin. You can use a dermatoscope to observe any changes in their size, shape, color, or texture, and promptly visit a hospital for examination if there are any abnormalities.






















