Article
Dermoscopy Squamous Cell Carcinoma
Skin cancer is one of the common malignant tumors in human beings, and although the incidence rate is relatively low in our country, it is a common malignant tumor in the white race and shows a rising trend. If skin cancer is not detected and treated early, it may pose a threat to the patient’s…
Skin cancer is one of the common malignant tumors in human beings, and although the incidence rate is relatively low in our country, it is a common malignant tumor in the white race and shows a rising trend. If skin cancer is not detected and treated early, it may pose a threat to the patient’s life. Squamous cell carcinoma of the skin is a malignant tumor derived from the keratin-forming cells of the epidermis. Tumors occurring in the ear, preauricular skin, or mucocutaneous junction tend to be more aggressive.
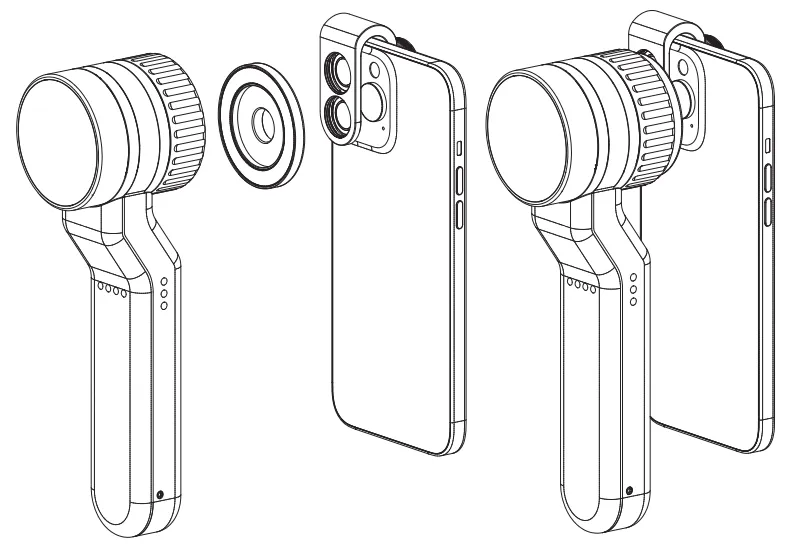
Dermoscopy, is a powerful diagnostic tool for dermatologists as it provides clear images of microscopic structures that are difficult to visualize with the naked eye, such as the living epidermis and the papillary layer of the dermis.
Clinical Features of Squamous Cell Carcinoma
According to histologic classification, squamous cell carcinoma of the skin can be divided into three main types: highly differentiated squamous cell carcinoma, moderately differentiated squamous cell carcinoma, and poorly differentiated squamous cell carcinoma. Squamous cell carcinoma of the skin usually presents as plaques, nodules, or wart-like lesions and shows cauliflower-like growths on the surface, which are sometimes covered by a scab that subsequently sloughs off to form an ulcer.
Prolonged exposure to ultraviolet light is one of the most important factors leading to squamous cell carcinoma. UV rays can cause DNA damage to skin cells, triggering genetic mutations that can lead to cancer. Therefore, long-term outdoor workers are at high risk for squamous cell carcinoma of the skin.

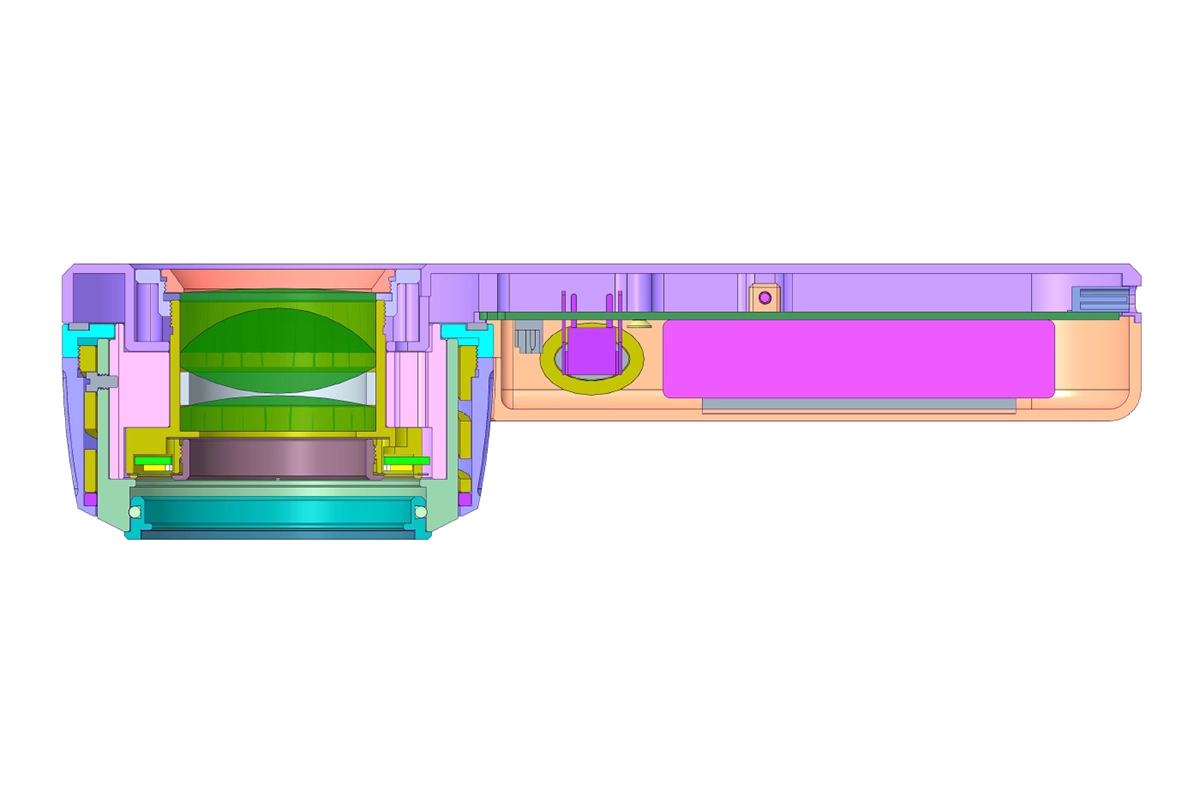
Principles and Methods of Dermoscopy
Dermatoscope is a kind of skin microscope that can magnify dozens of times, through the principle of optical magnification, it can observe the subtle pigment and vascular structural changes in the deeper layers of the skin that cannot be observed by the naked eye. Before starting the dermoscopy, the skin surface to be examined is cleaned to ensure that it is free of oil, followed by applying the probe of the dermoscopy to the skin surface to be observed. Maintain a good distance between the probe and the skin and adjust the focus until the image is clear.
Dermoscopy has a wide range of indications, including but not limited to the following: skin tumors, pigmented dermatoses, inflammatory dermatoses, erythematous papulosquamous diseases. However, dermoscopy is mainly used as an aid in the diagnosis of disease and cannot directly treat the disease. The results of dermoscopy need to be further confirmed by biopsy results.
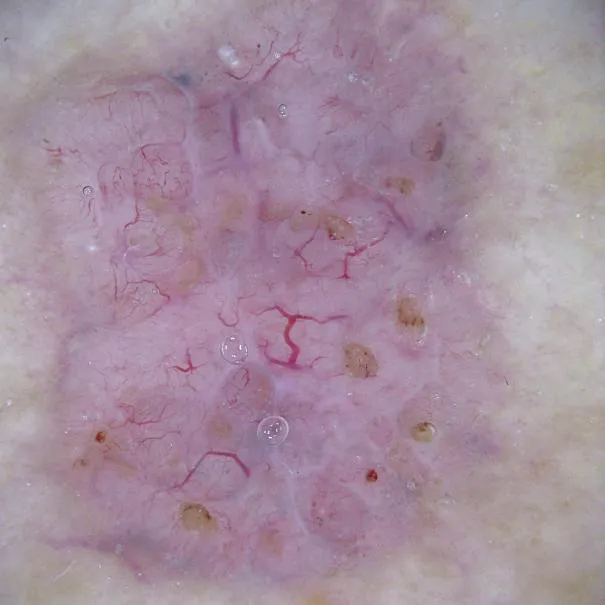
Dermoscopic Features of Squamous Cell Carcinoma of the Skin
Squamous cell carcinoma of the skin is a common malignant tumor of the skin, which usually appears dermoscopically as small, hard, red nodules that may evolve into warty or papillomatous forms with a scaly surface and a central, ulcer-prone area. Squamous cell carcinoma of the skin is usually classified clinically into several types, each with different microscopic features.
Nodular ulcerated type: waxy, shiny, discoid plaques that tend to knit together in the center with brown, yellow-brown, or dark gray scarring. The edges of the ulcers are firm and rolled up, often translucent and bumpy, with a pearly or waxy appearance at the base.
Pigmented: The damage is the same as that of the nodular ulcer type, but contains more pigment, as well as dotted or reticulated dark brown or dark brown pigmented spots, and hyperpigmentation in the central area.
Fibrotic type: hard yellowish or yellowish-white plaques, slightly elevated, with unclear borders, resembling scleroderma.
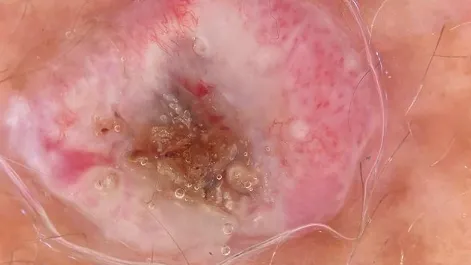
Dermoscopy in the Diagnosis of Squamous Cell Carcinoma of the Skin
Value in Early Diagnosis Dermoscopy, as a non-invasive, non-invasive, painless and advanced skin imaging diagnostic tool, has the advantage of high diagnostic accuracy.
Dermoscopy can provide detailed information on the morphology, surface structure and pigmentation of skin lesions, which helps to determine the nature and type of lesions. Histopathological examination, on the other hand, is the result of tissue biopsy and cytological examination, which can determine the type and severity of pathology by analyzing the morphological, structural and functional changes of tissues or cells.
In practice, dermoscopy and histopathology are often complementary. Dermoscopy can be used as an initial screening tool, while histopathology, as the gold standard, can further confirm the accuracy of dermoscopy.
Significance of Dermoscopy
Traditional methods of examining skin diseases require taking samples or performing other invasive procedures that inevitably cause pain to the patient. Dermoscopy, as a non-invasive method, avoids these pains and increases patient comfort. In the treatment of skin tumors, dermoscopy can assist in determining the tumor boundaries and provide guidance for surgical excision. This helps doctors to remove the lesions more precisely and reduce surgical trauma and complications.
After surgery, doctors can also use dermoscopy to regularly observe the patient’s skin disease and predict the patient’s risk of recurrence. This allows doctors to develop a more rational follow-up plan for patients to detect and manage recurrences in a timely manner.

New Technologies and Future Directions in Dermatoscopy
The application of reflection confocal microscopy (RCM) and artificial intelligence in dermatoscopy image analysis is an important progress in the field of dermatological medical imaging, and they will surely become the future mainstream research direction of dermatoscopy in the future.RCM uses laser as a monochromatic light source, and it can penetrate and image the skin at different depths by adjusting the wavelength of the light source and the laser power. And artificial intelligence, through the training of a large amount of image data, will be able to automatically extract, identify and classify diseased tissues in dermoscopy images in the future.
The Importance of Dermoscopy in the Diagnosis of Squamous Cell Carcinoma
Dermoscopy can observe the subtle morphology, size, color, and vascularity of squamous cells of the skin, which can help doctors better determine the degree of progression of a patient’s disease and thus better formulate a treatment plan for the patient. However, the results of dermoscopy and diagnosis are highly dependent on the doctor’s expertise and experience. Doctors need to have an in-depth understanding of dermoscopic images in order to accurately determine the nature of a lesion.
Dermatologists should continue to learn the latest dermoscopic techniques and research results, and through continuous clinical practice, improve their mastery of dermoscopic techniques and increase the accuracy of their judgment of various common skin diseases. In addition, the use of dermoscopy as a routine means of screening and diagnosis of squamous cell carcinoma of the skin is conducive to the early treatment and rehabilitation of patients.
Recommended reading
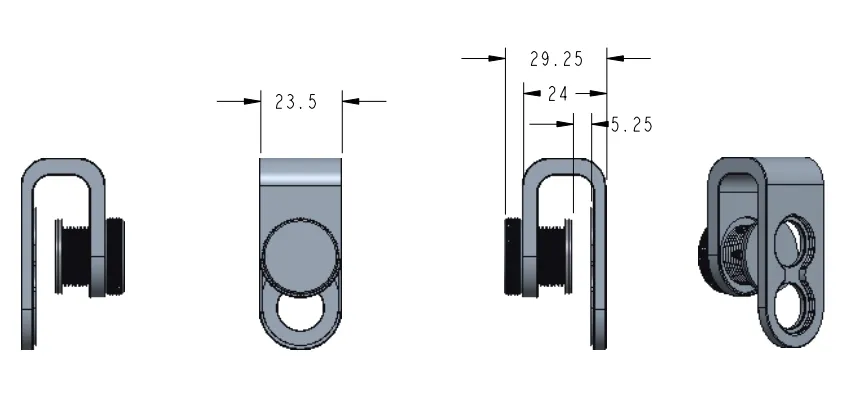
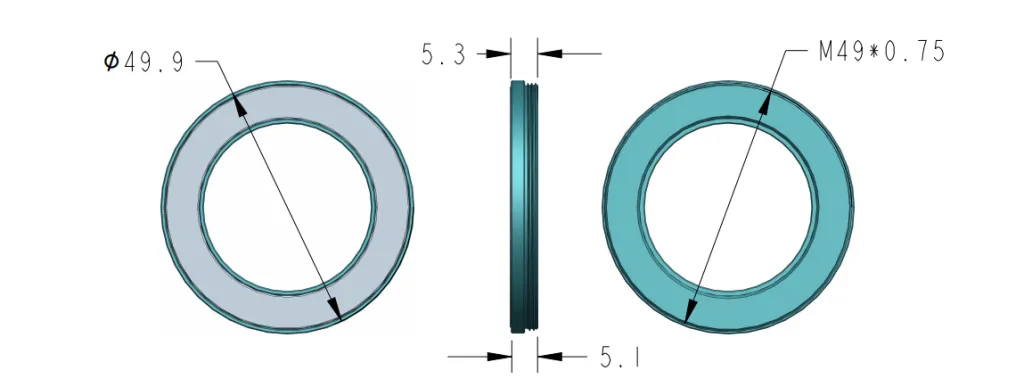
Leading China Products Supply Making Lightweight Professional Dermoscopy of Psoriasis - IBOOLO
As a premier dermoscopy of psoriasis products supply in China, over 11+ years we have perfected Professional models balancing professional-level HD magnification in a lightweight body for convenient use.
Dermoscopy of Dermatofibroma – IBOOLO
A dermatofibroma is a common benign bump in the skin.Dermatofibroma is usually harmless and typically appears on the lower legs. Dermatofibroma is easily mistaken from other skin tumors due to its appearance. This brings much difficult to diagnose. Hence, how to exactly diagnose dermatofibroma is special important to dermatology filed. What is dermatofibroma...
China Manufacturer & Factory Specializing in Professional Dermoscopy Models - IBOOLO
Through engineering mastery nurtured over a decade, our China manufacturer & factory produces Professional dermoscopy devices combining sturdy builds and unmatched optics for flexible precision skin analysis.