Article
Skin Lesions Under IBOOLO DE-3100 Dermoscope
The DE-3100 is the first handheld optical dermatoscope launched by IBOOLO. It is a fully functional and highly practical dermatoscope. Why You Should Buy the IBOOLO DE-3100? The IBOOLO DE-3100 features a full aluminum housing design, making it highly durable and robust. It offers multiple lighting modes—including polarized light, non-polarized light, and amber polarized light—suitable…
The DE-3100 is the first handheld optical dermatoscope launched by IBOOLO. It is a fully functional and highly practical dermatoscope.
Why You Should Buy the IBOOLO DE-3100?
The IBOOLO DE-3100 features a full aluminum housing design, making it highly durable and robust. It offers multiple lighting modes—including polarized light, non-polarized light, and amber polarized light—suitable for observing various types of skin lesions. With 10X magnification, it delivers excellent image clarity and detail. The device is priced at only 499 USD, and IBOOLO provides a two-year warranty. During this period, we offer free repair or replacement services for any product quality issues. In addition, if you encounter any questions or difficulties while using the device, our technical support team provides free professional consultation.
The following skin lesions were all photographed with the DE-3100 connected to a phone.
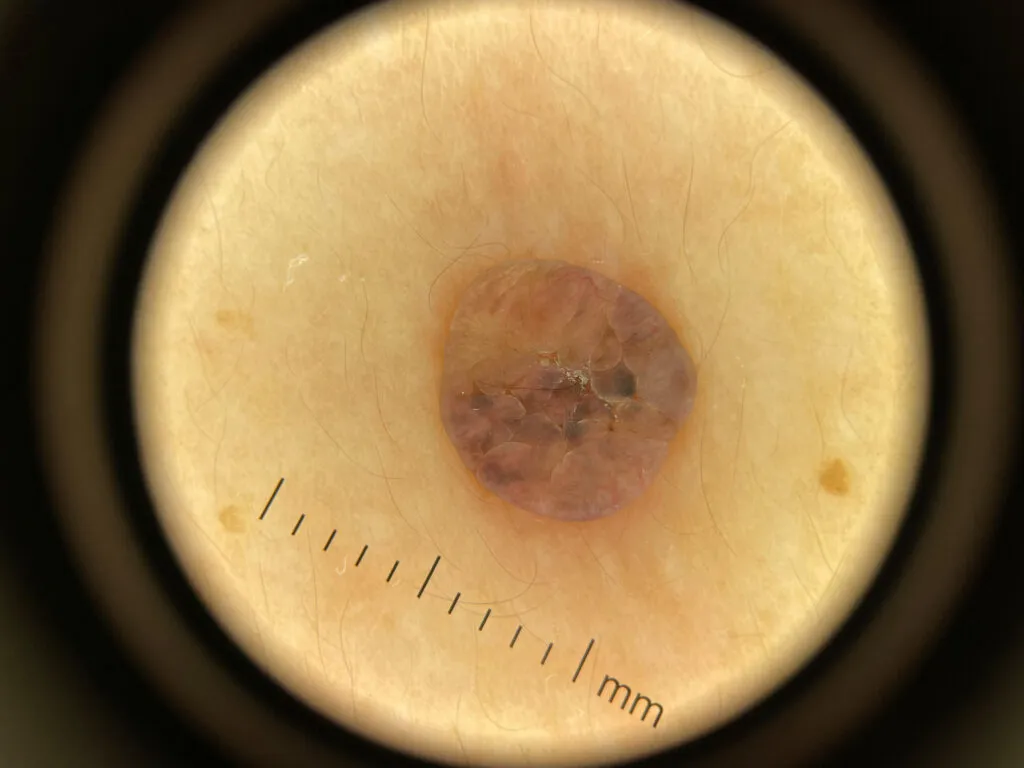
Dermatofibroma under IBOOLO DE-3100
Dermatofibroma often demonstrates a characteristic dermoscopic appearance that aids in distinguishing it from other benign or malignant lesions. The most consistent finding is a central whitish, scar-like area or a white patch surrounded by a delicate, thin, and regular peripheral pigment network. This central white zone corresponds histologically to fibrosis within the dermis. Additional findings may include peripheral light to dark brown pigmentation, dotted or linear vessels, and, in hemosiderotic variants, bluish or grayish homogeneous areas due to hemosiderin deposition.
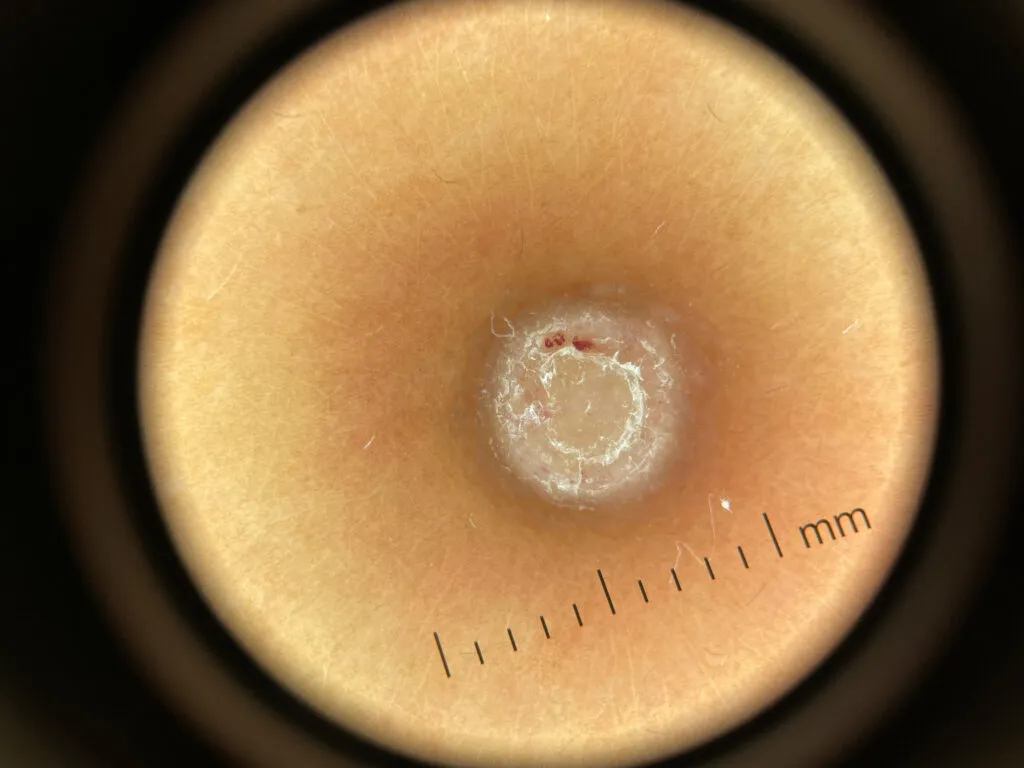
Intradermal nevus under IBOOLO DE-3100
Intradermal nevus typically shows a dermoscopic pattern that lacks a regular pigment network. The lesion often appears skin-colored or light brown and may be papillomatous or dome-shaped. The global dermoscopic pattern is commonly globular or cobblestone-like, with uniform round to oval brown globules that correspond to nests of melanocytes within the dermis. Fine telangiectatic vessels or comma vessels may be observed, especially in raised lesions. Terminal hairs may emerge from the surface, and structureless pale areas are common, reflecting dermal maturation.

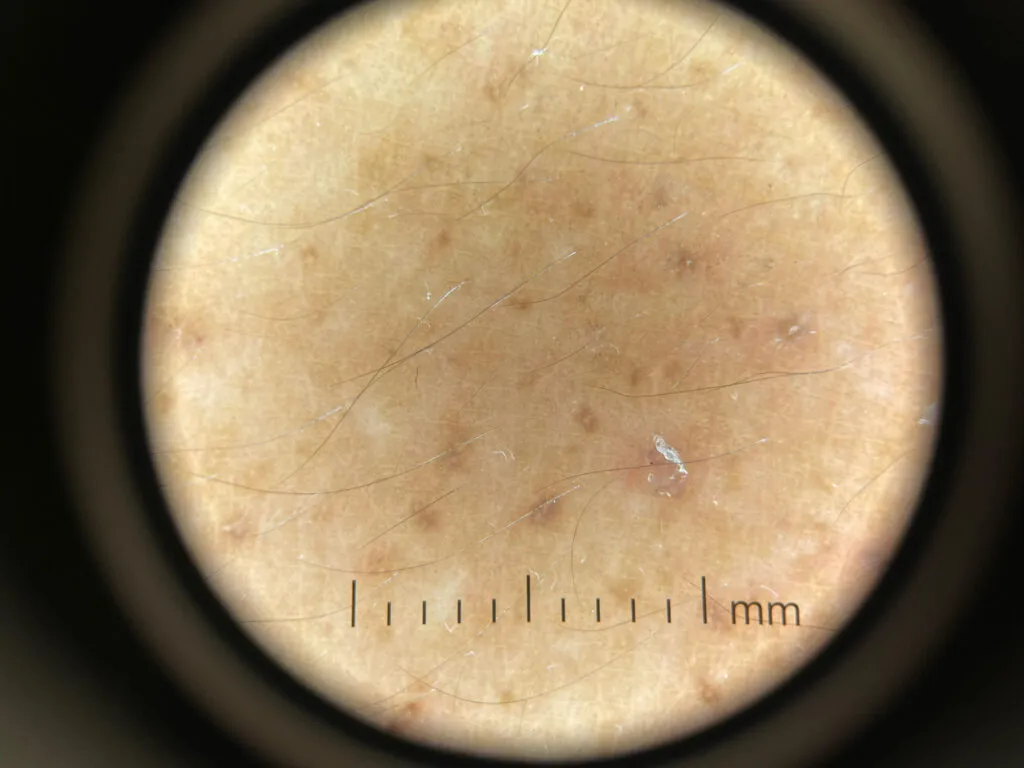
Junctional nevus under IBOOLO DE-3100
Junctional nevus displays a regular pigment network that is symmetric and uniform in color and line thickness. The network is typically evenly distributed across the lesion and sharply demarcated from the surrounding skin. The background color ranges from light to dark brown depending on melanin density. Dots and globules may be present but usually remain uniform in size and distribution.

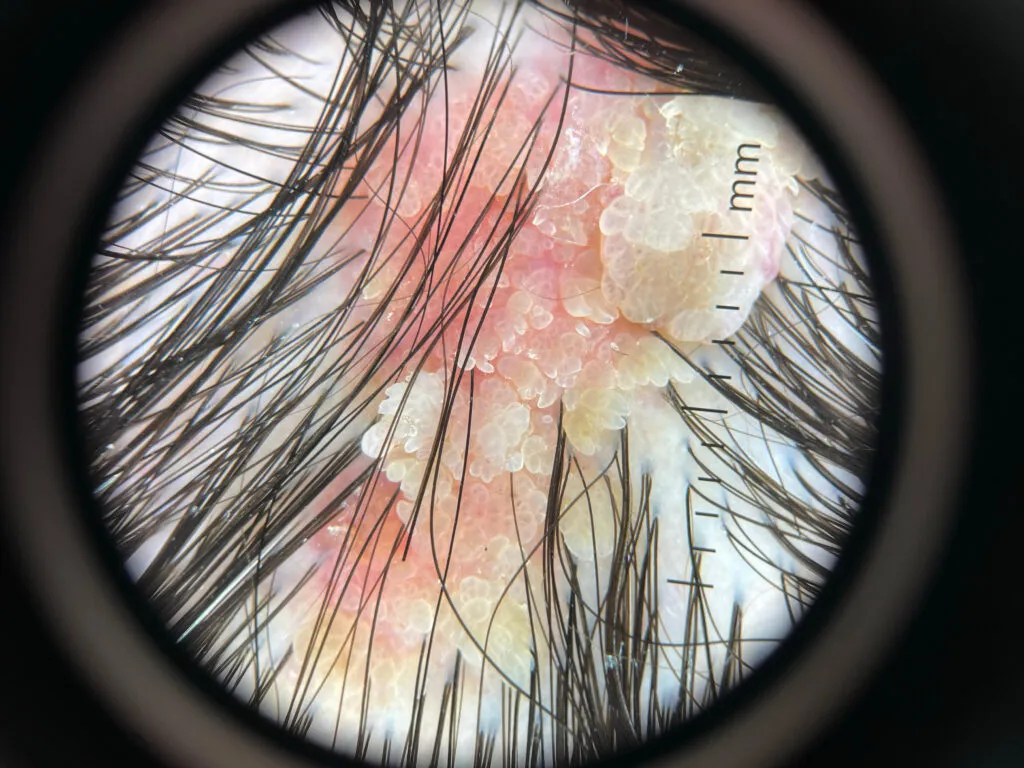
Sebaceous nevus under IBOOLO DE-3100
Sebaceous nevus exhibits dermoscopic findings that evolve with age. In early childhood, the lesion often appears as yellowish, structureless areas with subtle lobular or homogeneous yellow-orange coloration corresponding to sebaceous gland proliferation. In adolescence or adulthood, the surface becomes verrucous, showing a cerebriform or papillomatous pattern with yellow globules, clods, and sometimes branching vessels or whitish areas of fibrosis. These changes reflect maturation and possible secondary adnexal tumor development.

Cutaneous amyloidosis under IBOOLO DE-3100
Cutaneous amyloidosis—including macular and lichen types—shows distinctive pigment patterns under dermoscopy. A central whitish or brown hub is commonly seen, surrounded by fine, radiating brown streaks or a reticulated pigment network, producing a “hub-and-spoke” or “rippled” pattern. This corresponds to amyloid deposits in the papillary dermis with reactive melanocytic hyperpigmentation at the basal layer. Perifollicular pigmentation and fine scaling may also be observed.
Epidermal nevus under IBOOLO DE-3100
Epidermal nevus, particularly the verrucous type, demonstrates dermoscopic features reflecting epidermal hyperplasia. Typical findings include thick brown circles, branched brown lines, and brown dots arranged in linear or serpiginous patterns. White or yellowish papillary structures may be visible, with fine or adherent scaling. Dotted or short linear vessels can also appear, corresponding to papillomatosis and hyperkeratosis seen histologically.
Persistent nevus under IBOOLO DE-3100
Dermoscopically, persistent nevi commonly show asymmetric but limited pigmentation patterns, with areas of light to dark brown color distributed irregularly over a whitish or pink scar background. The pigment network, when present, often appears broken, incomplete, or confined within the borders of the scar. Radial lines and globules may be seen, but they generally remain centrally located and do not extend beyond the scar’s margin. Fine linear or dotted vessels can also appear due to reactive vascular proliferation in the healing dermis. These characteristics contrast with recurrent melanoma, where pigmentation often extends beyond the scar edge, displays greater color variability including gray, blue, or black tones, and exhibits atypical network structures.

Seborrheic keratosis under IBOOLO DE-3100
The most consistent dermoscopic findings include multiple milia-like cysts, comedo-like openings, and fissures and ridges forming a brain-like or cerebriform surface pattern. The lesion surface often shows sharply demarcated borders with a waxy or keratotic appearance, correlating histologically with hyperkeratosis and acanthosis. Colors range from light brown to dark brown or black, depending on the thickness of the keratin and degree of pigmentation. In non-pigmented or lightly pigmented lesions, yellowish or whitish structureless areas may be observed. Some lesions show a network-like or reticular pattern, but this is usually pseudonetwork-like, caused by follicular openings rather than a true pigment network.