Article
Skin Lesions Under IBOOLO DE-4100 Dermoscope
This article mainly aims to share a series of lesion images captured by users with the IBOOLO DE-4100 dermatoscope. The IBOOLO DE-4100 offers four lighting modes: polarized light, non-polarized light, amber light, and polarized-amber mixed light. The images presented in this article were primarily taken using the polarized mode. Basal Cell Carcinoma under IBOOLO DE-4100 On…
This article mainly aims to share a series of lesion images captured by users with the IBOOLO DE-4100 dermatoscope. The IBOOLO DE-4100 offers four lighting modes: polarized light, non-polarized light, amber light, and polarized-amber mixed light. The images presented in this article were primarily taken using the polarized mode.
Basal Cell Carcinoma under IBOOLO DE-4100
On dermoscopy, basal cell carcinoma (BCC) is characterized by the absence of a pigment network and the presence of specific structures such as arborizing telangiectasias, blue-gray ovoid nests, maple-leaf–like areas, spoke-wheel areas, and ulceration. Polarized light can reveal shiny white structures, and in superficial BCC, short fine telangiectasias and multiple small erosions are common.

Melanoma under IBOOLO DE-4100
Melanoma under dermoscopy typically displays asymmetry and an atypical pigment network, often accompanied by irregular dots and globules, streaks or pseudopods, and the presence of a negative network. Additional features include blue-white veil, regression structures such as peppering and scar-like depigmentation, shiny white structures, and polymorphous or atypical vessels. These features, particularly shiny white structures, pseudopods, irregular pigmentation, blue-white veil, and peppering, are strongly associated with melanoma diagnosis.

Actinic Keratosis under IBOOLO DE-4100
Actinic keratosis exhibits the so-called strawberry pattern: a pink-to-red background surmounted by a white-yellow surface scale arranged in a geometric, tile-like fashion. Under polarised light, fine wavy hairpin vessels are often visible, and rosettes—four white dots arranged in a square—may be seen. The scale is adherent and cannot be removed without trauma, distinguishing the lesion from seborrhoeic keratosis.

Cherry Angioma under IBOOLO DE-4100
Cherry angioma, a common type of acquired hemangioma, shows a distinctive lacunar pattern under dermoscopy. This consists of well-demarcated, round to oval, red, maroon, or blue-black lacunae separated by fibrous septa. Thrombosed areas may appear darker, and the lacunar arrangement is considered diagnostic.

Spider Angioma under IBOOLO DE-4100
Spider angioma, also known as spider telangiectasis, is characterized by a central red arteriole with radially arranged thin capillaries. On dermoscopy, the blanch-and-refill sign is diagnostic: pressure applied to the central vessel causes blanching of the entire lesion, with rapid refill upon release. This pattern reflects the vascular structure of the lesion.

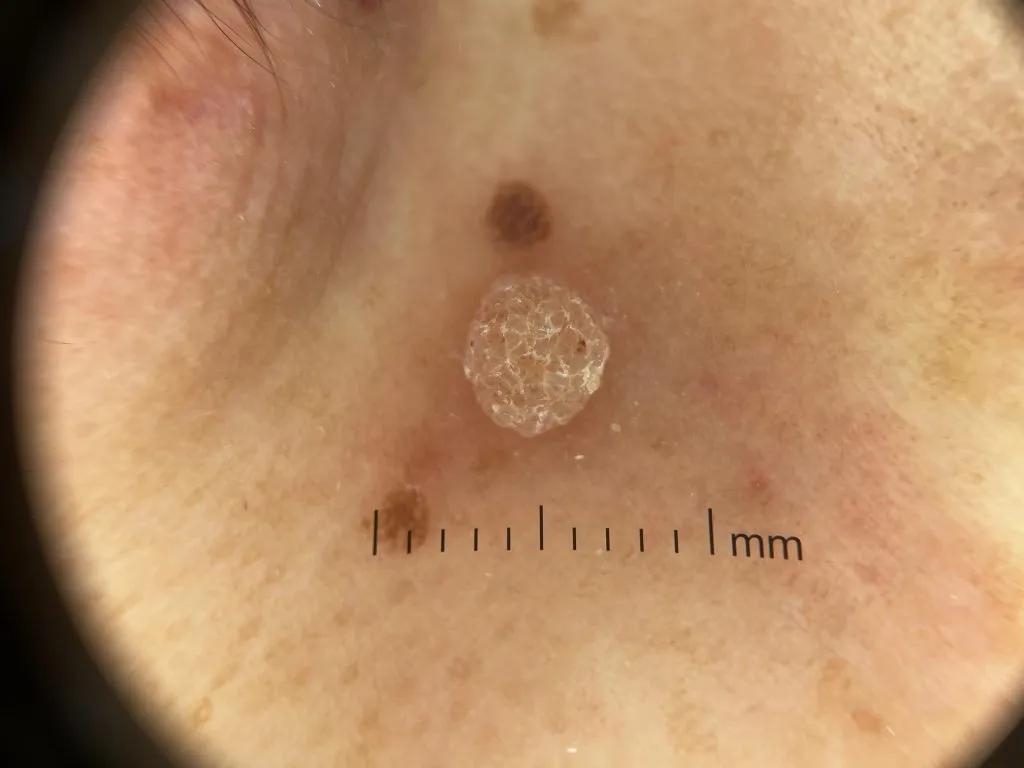
Common Wart under IBOOLO DE-4100
Common wart shows a papillomatous, hyperkeratotic surface on dermoscopy, often with multiple densely packed papillae. Each papilla contains a central red or black dot or loop corresponding to thrombosed capillaries. The skin lines are interrupted, and plantar warts frequently display numerous hemorrhagic dots within a yellowish papilliform surface, which helps differentiate them from calluses or corns.
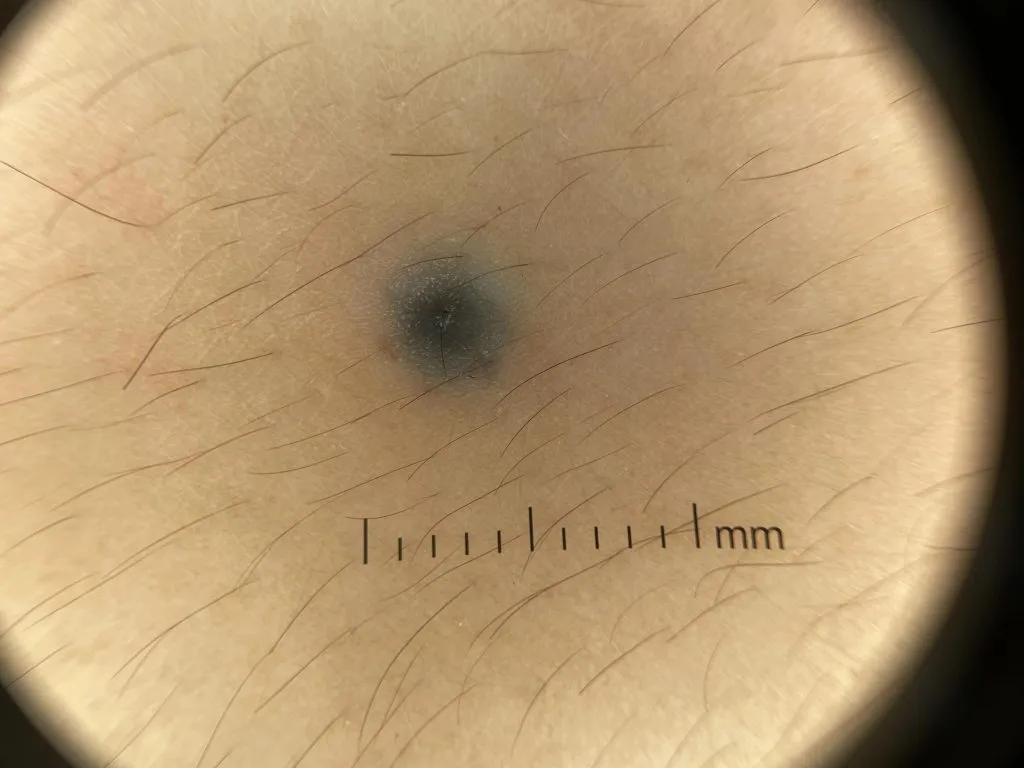
Blue Nevus under IBOOLO DE-4100
A blue nevus under dermoscopy typically shows uniform, structureless pigmentation that appears steel-blue, blue-gray, blue-brown, or blue-black; this homogeneous blue appearance is the hallmark feature, and in some cases small dots or globules may also be observed or rare depigmented scarlike areas peripherally.
Sebaceous Nevus under IBOOLO DE-4100
A sebaceous nevus during dermoscopic examination frequently reveals aggregated yellowish or brown globules and lobular structures on a yellow background. In childhood, these features appear as clustered lobules in yellow background; verrucous or warty stages show whitish-yellow lobular or grayish papillary appearance, while nodular stages may display homogeneous yellow–whitish pigmentation.

Verrucous Epidermal Nevus under IBOOLO DE-4100
A verrucous epidermal nevus demonstrates a mix of distinctive dermoscopic structures. Common findings include large brown circles (oval or round structures with darker brown edges surrounding lighter areas), thick branched brown lines, brown dots and globules arranged in lines or serpiginous patterns, exophytic white and brown papillary structures, cerebriform or cobblestone patterns, thick adherent scales, and dotted vessels; these features may overlap with seborrheic keratosis, but the presence of cerebriform pattern and large brown circles may be particularly specific to this nevus.

Seborrheic Keratosis under IBOOLO DE-4100
Seborrheic keratosis exhibits multiple, well-characterized dermoscopic signs. These include milia-like cysts, comedo-like (pseudohorn) openings, fissures and ridges often describing a cerebriform or “gyri and sulci” pattern, moth-eaten or sharply demarcated borders, fingerprint-like structures, “fat-finger” projections, and hairpin (looped) vessels often surrounded by a whitish halo.

Acral Junctional Nevu under IBOOLO DE-4100
An acral junctional nevus—interpreted as a benign melanocytic nevus arising at the border of acral skin such as the sole—displays under dermoscopy patterns typical of benign acral melanocytic nevi. These include the parallel furrow pattern (pigmentation following the skin sulci), lattice-like pattern (pigmentation along furrows with crossing linear bands), fibrillar pattern (fine streaks crossing dermatoglyphic ridges, often due to pressure), homogeneous pattern, or globular variants; among these, parallel furrow is the prototypical sign of benignity, and fibrillar and lattice-like variants may also appear, sometimes mixed within the same lesion.

Café-au-lait Macule under IBOOLO DE-4100
A café-au-lait macule under dermoscopy shows a uniform light-brown background with a faint but consistently reticulated brown pigment network; in early lesions, this may appear as focal thickening of the network forming tiny arcuate lines, while in darker or more mature lesions the pigment network becomes uniformly thickened and more evident. These lesions lack structures such as dots, globules, streaks, or vascular patterns that are typically seen in melanocytic or vascular conditions, distinguishing café-au-lait macules from nevi or melanomas.























